Predictors of Visit Frequency for Patients Using Ongoing Chiropractic Care for Chronic Low Back and Chronic Neck Pain; Analysis of Observational Data
SOURCE: BMC Musculoskeletal Disorders 2020 (May 13); 21 (1): 298
Patricia M. Herman, PhD, Sarah E. Edgington, PhD, Eric L. Hurwitz, DC, PhD, & Ian D. Coulter, PhD
RAND Corporation,
Santa Monica, CA, USA.
Background: Chronic spinal pain is prevalent, expensive and long-lasting. Several provider-based nonpharmacologic therapies have now been recommended for chronic low-back pain (CLBP) and chronic neck pain (CNP). However, healthcare and coverage policies provide little guidance or evidence regarding the long-term use of this care. To provide one glimpse into the long-term use of nonpharmacologic provider-based care, this study examines the predictors of visit frequency in a large sample of patients with CLBP and CNP using ongoing chiropractic care.
Methods: Observational data were collected from a large national sample of chiropractic patients in the US with non-specific CLBP and CNP. Visit frequency was defined as average number of chiropractic visits per month over the 3-month study period. Potential baseline predictor variables were entered into two sets of multi-level models according to a defined causal theory-in this case, Anderson’s Behavioral Model of Health Services Use.
Results: Our sample included 852 patients with CLBP and 705 with CNP. Visit frequency varied significantly by chiropractor/clinic, so our models controlled for this clustering. Patients with either condition used an average of 2.3 visits per month. In the final models visit frequency increased (0.44 visits per month, p = .008)
There are more articles like this @ our:
LOW BACK PAIN Page and the:
for those with CLBP and some coverage for chiropractic, but coverage had little effect on visits for patients with CNP. Patients with worse function or just starting care also had more visits and those near to ending care had fewer visits. However, visit frequency was also determined by the chiropractor/clinic where treatment was received. Chiropractors who reported seeing more patients per day also had patients with higher visit frequency, and the patients of chiropractors with 20 to 30 years of experience had fewer visits per month. In addition, after controlling for both patient and chiropractor characteristics, the state in which care was received made a difference, likely through state-level policies and regulations.
Conclusions: Chiropractic patients with CLBP and CNP use a range of visit frequencies for their ongoing care. The predictors of these frequencies could be useful for understanding and developing policies for ongoing provider-based care.
KEYWORDS: Behavioral model of health services use; Chiropractic care; Chronic low back pain; Chronic neck pain; Visit frequency.
From the FULL TEXT Article:
Background
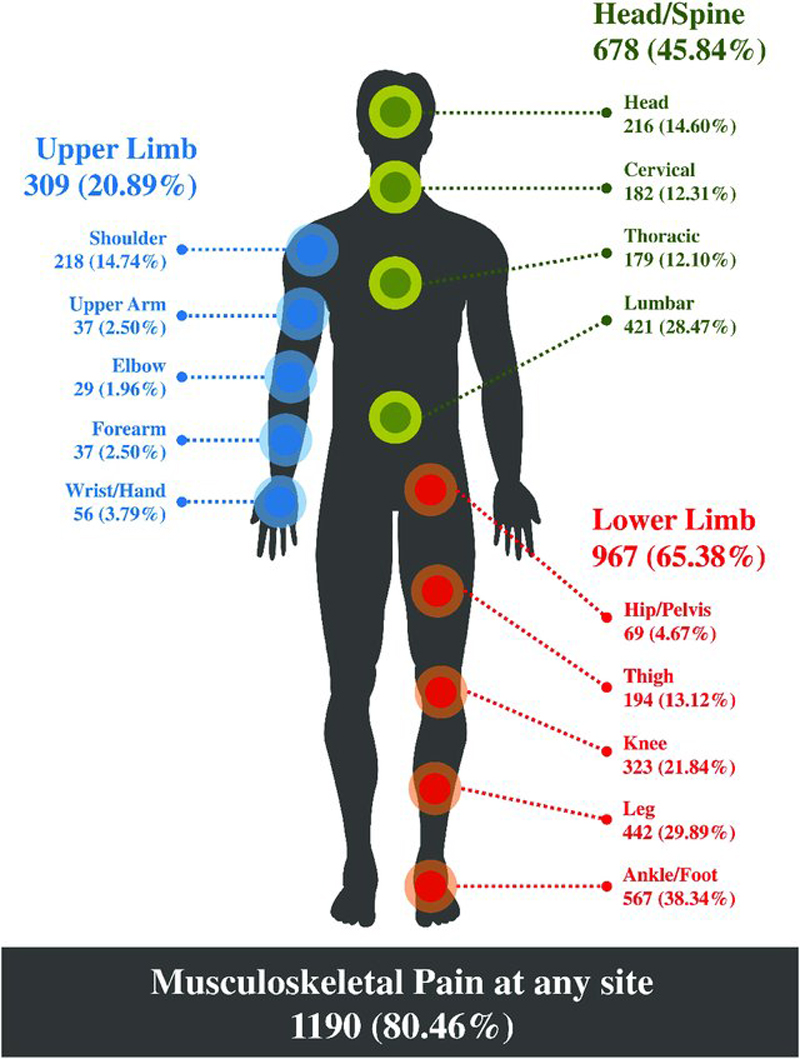
Chronic low-back pain (CLBP) and chronic neck pain (CNP) are the most common types of chronic pain, [1, 2] and their estimated combined adult prevalence is between 10 and 20% [1, 3–11]. This pain is associated with substantial co-morbidity, [12] and is expensive to the healthcare system [13] and to employers [14]. Chronic spinal pain is also long-lasting, with average pain durations from years to decades [15–19].
Many patients with CLBP and/or CNP use medications to manage their pain, including opioids [12, 20]. However, due to the dangers of opioid abuse, recent efforts have focused on finding effective nonpharmacologic therapies [21]. Guidelines now recommend a number of nonpharmacologic therapies for CLBP and CNP [22–24]. Several of these therapies (e.g., acupuncture, cognitive-behavioral therapy, multidisciplinary rehabilitation, spinal manipulation) require ongoing visits to providers.
Unfortunately, the ongoing long-term provision of provider-based care for chronic spinal pain, including appropriate visit frequencies, is not well-addressed in health and payer policies [25–27]. To some extent this is because many of these policies are based on a curative model [28, 29 ]— i.e., X number of treatments and you should be cured. These policies can require documentation of continued clinically meaningful improvement with the implication that treatment ends when a patients’ symptoms plateau at some maximum therapeutic benefit [30–35]. However, although many policies recognize that care beyond this plateau—i.e., chronic pain management [32] or ongoing or support care [35] — might be needed under certain conditions — e.g., if symptoms deteriorate with treatment withdrawal [30–32, 36] — little guidance and no evidence is offered for this care. This lack of information and support of ongoing pain management has been cited as one barrier to the use of recommended provider-based nonpharmacologic therapies for chronic spinal pain [37].
Information on how patients with CLBP and CNP utilize ongoing provider-based nonpharmacologic care may be useful to the development of better policies in support of this care. It is estimated that 30% of patients with spinal pain have visited a chiropractor, one type of recommended provider-based nonpharmacologic care [38]. In particular, it would be useful to examine the treatment frequency patients used, and the determinants of those frequencies. These determinants include patient characteristics but may also include characteristics of the treating chiropractors.
This study took advantage of data gathered from a large national sample of patients with CLBP and CNP who were using chiropractic care [15]. Other analyses of these data have shown that this sample matches the age, gender, racial, ethnic, income and education levels seen in other national samples of chiropractic patients [15, 38–42]. It has also been shown that these patients have been in pain for an average of 14 years and have been using chiropractic care for an average of 11 years [15]. The majority have a goal of pain management (not cure) [43].
A study of their stated willingness-to-pay for pain reduction indicated that what they value is the maintenance of their current, generally mild pain levels, [44] and on average their symptoms over the 3-month study period are mild (average pain intensity of 3 and 4 on a 0–10 scale with minimal-to-moderate back dysfunction [45] and mild neck dysfunction [15, 46]) and may improve slightly [47]. This last may indicate that they have plateaued at maximum therapeutic benefit. However, on average these patients reported that their pain would double if they did not see their chiropractor, [15] which could be an indication of their experience with treatment withdrawals. In this study we examined the range of visit frequencies (visits/month) these patients used to determine the effect on this behavior of baseline insurance coverage, patient characteristics and the characteristics of the treating chiropractor.
Read the rest of this Full Text article now!





Leave A Comment