The Nordic Maintenance Care Program: Does Psychological Profile Modify the Treatment Effect of a Preventive Manual Therapy Intervention? A Secondary Analysis of a Pragmatic Randomized Controlled Trial
SOURCE: PLoS One. 2019 (Oct 10); 14 (10): e0223349
Andreas Eklund ,Irene Jensen,Charlotte Leboeuf-Yde,Alice Kongsted,Mattias Jonsson, Peter Lövgren,Jakob Petersen-Klingberg,Christian Calvert,Iben Axén
Karolinska Institutet,
Institute of Environmental Medicine,
Unit of Intervention and Implementation Research for Worker Health,
Stockholm, Sweden.
|
A recent single blinded placebo controlled study, conducted by the Mansoura Faculty of Medicine, conclusively demonstrates that maintenance care provides significant benefits for those with chronic low back pain. |
BACKGROUND: Chiropractic maintenance care is effective as secondary/tertiary prevention of non-specific low back pain (LBP), but the potential effect moderation by psychological characteristics is unknown. The objective was to investigate whether patients in specific psychological sub-groups had different responses to MC with regard to the total number of days with bothersome pain and the number of treatments.
METHOD: Data from a two-arm randomized pragmatic multicenter trial with a 12–month follow up, designed to investigate the effectiveness of maintenance care, was used. Consecutive patients, 18–65 years of age, with recurrent and persistent LBP seeking chiropractic care with a good effect of the initial treatment were included. Eligible subjects were randomized to either maintenance care (prescheduled care) or to the control intervention, symptom-guided care.
There are more articles like this @ our:
The primary outcome of the trial was the total number of days with bothersome LBP collected weekly for 12 months using an automated SMS system. Data used to classify patients according to psychological subgroups defined by the West Haven-Yale Multidimensional Pain Inventory (adaptive copers, interpersonally distressed and dysfunctional) were collected at the screening visit.
RESULTS: A total of 252 subjects were analyzed using a generalized estimating equations linear regression framework. Patients in the dysfunctional subgroup who received maintenance care reported fewer days with pain (–30.0; 95% CI: –36.6, –23.4) and equal number of treatments compared to the control intervention. In the adaptive coper subgroup, patients who received maintenance care reported more days with pain (10.7; 95% CI: 4.0, 17.5) and more treatments (3.9; 95% CI: 3.5, 4.2). Patients in the interpersonally distressed subgroup reported equal number of days with pain (–0.3; 95% CI: –8.7, 8.1) and more treatments (1.5; 95% CI: 0.9, 2.1) on maintenance care.
CONCLUSIONS: Psychological and behavioral characteristics modify the effect of MC and should be considered when recommending long-term preventive management of patients with recurrent and persistent LBP.
TRIAL REGISTRATION Clinical trials.gov; NCT01539863
From the Full-Text Article:
Introduction
Non-specific low back pain (LBP) is a highly prevalent condition, affecting a large part of the population with major consequences. [1, 2] For a highly disabling recurrent and costly condition it seems logical to invest in preventive strategies to mitigate and minimize its impact on the individual and on society. [3–6] However, the evidence for effective interventions aimed at preventing LBP is limited. To date, only exercise, exercise in combination with education and pre-planned manual treatment (chiropractic maintenance care, MC) have been shown to be effective. [7, 8]
MC has traditionally been used by chiropractors and is described as a long-term management strategy, introduced when treatment benefit has been recorded after an initial care plan, with the aim of preventing future episodes and deterioration by treating the patient regularly irrespective of symptoms. [9–14] Ninety-eight percent of all Swedish chiropractors support the concept of MC and consider it to be a useful clinical procedure, at least in some circumstances. [9] MC is mainly used as a form of secondary or tertiary prevention aimed at recurrent and persistent conditions. [9, 12, 15–17] There seems to be a common patient-oriented management concept among chiropractors according to which patients are selected for MC mainly on the basis of their previous history of pain and the effectiveness of the initial care plan. [10, 12, 15–20] In previous studies, the proportion of chiropractic MC visits ranged between 14% and 41%. [10, 13, 14, 20–22] However, the evidence for its effectiveness and clinical usefulness have been lacking until recently. [8, 11] Previous research has been either efficacy studies or designed with little consideration of how MC is delivered in clinical practice. [23–26]
In a comprehensive program starting 2008, the Nordic Maintenance Care Program, indications, content and frequency of MC have been systematically investigated by Scandinavian researchers. [10, 12, 15–20] Based on this knowledge, a randomized pragmatic clinical trial was designed to investigate the effectiveness of MC for recurrent and persistent LBP. [27]
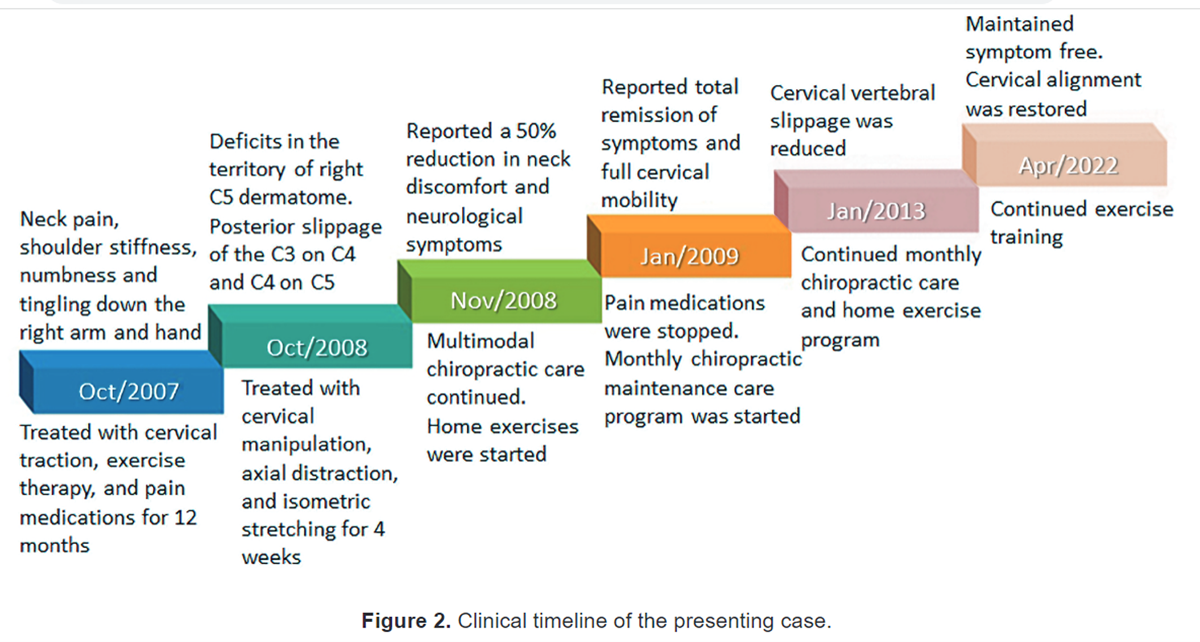
The trial found that the MC group had 12.8 fewer days with bothersome LBP (95% CI: 10.1, 15.5) over a year compared to the control group, who had treatments with a similar content but only when symptoms reappeared. [8] Although more effective, the number of visits was also somewhat higher in the MC group: 6.7 treatments (95% CI = 6.6, 6.8) compared to 4.8 treatments (95% CI = 4.7, 4.9) during the 52–week study period. A large variability in the outcomes within treatment groups suggested that there might be sub-groups of patients who responded better to MC than others.
Psychological [28, 29], behavioral [30] and social characteristics [31] of LBP patients are known to be important prognostic factors in the transition from acute to persistent pain states. [32–35] Based on the cognitive-behavioral conceptualization of pain, the Swedish version of the West Haven-Yale multidimensional pain inventory (MPI-S) has been shown to capture and measure the psychological and behavioral dimensions of the chronic pain experience. [36]
Read the rest of this Full Text article now!



Leave A Comment