A Scoping Review of Biopsychosocial Risk Factors and Co-morbidities for Common Spinal Disorders
SOURCE: PLoS One. 2018 (Jun 1); 13 (6):e0197987
Bart N. Green, Claire D. Johnson, Scott Haldeman, Erin Griffith, Michael B. Clay, Edward J. Kane, Juan M. Castellote, Shanmuganathan Rajasekaran, Matthew Smuck, Eric L. Hurwitz, Kristi Randhawa, Hainan Yu, Margareta Nordin
Qualcomm Health Center,
Stanford Health Care,
San Diego, California
OBJECTIVE: The purpose of this review was to identify risk factors, prognostic factors, and comorbidities associated with common spinal disorders.
METHODS: A scoping review of the literature of common spinal disorders was performed through September 2016. To identify search terms, we developed 3 terminology groups for case definitions: 1) spinal pain of unknown origin, 2) spinal syndromes, and 3) spinal pathology. We used a comprehensive strategy to search PubMed for meta-analyses and systematic reviews of case-control studies, cohort studies, and randomized controlled trials for risk and prognostic factors and cross-sectional studies describing associations and comorbidities.
RESULTS: Of 3,453 candidate papers, 145 met study criteria and were included in this review. Risk factors were reported for group 1: non-specific low back pain (smoking, overweight/obesity, negative recovery expectations), non-specific neck pain (high job demands, monotonous work); group 2: degenerative spinal disease (workers’ compensation claim, degenerative scoliosis), and group 3: spinal tuberculosis (age, imprisonment, previous history of tuberculosis), spinal cord injury (age, accidental injury), vertebral fracture from osteoporosis (type 1 diabetes, certain medications, smoking), and neural tube defects (folic acid deficit, anti-convulsant medications, chlorine, influenza, maternal obesity). A range of comorbidities was identified for spinal disorders.
There are more articles like this @ our:
CONCLUSION: Many associated factors for common spinal disorders identified in this study are modifiable. The most common spinal disorders are co-morbid with general health conditions, but there is a lack of clarity in the literature differentiating which conditions are merely comorbid versus ones that are risk factors. Modifiable risk factors present opportunities for policy, research, and public health prevention efforts on both the individual patient and community levels. Further research into prevention interventions for spinal disorders is needed to address this gap in the literature
From the FULL TEXT Article
Introduction
Spinal disorders include a wide range of musculoskeletal problems affecting the spinal column and associated structures. [1] These disorders are common reasons for patients of all ages and socioeconomic status to seek health care and are a substantial cause of morbidity, disability, and suffering. The prevalence of these disorders has risen sharply since 1990 and they are a leading cause of global years lived with disability. [2] To address these burdens, it would be beneficial to identify risk factors for the most common spinal disorders to inform policy makers and future research efforts of potential public health interventions that might address these risk factors.
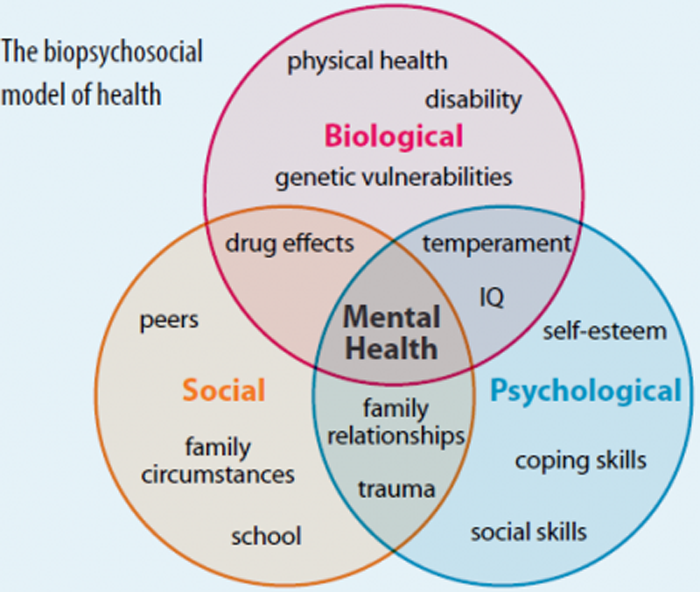
Spinal disorders should be considered as components of a more complex biopsychosocial model of health and not in isolation. Population-based studies have suggested that some spinal conditions may be associated with health behaviors, such as smoking [3, 4], high body mass index [5, 6], and insufficient physical activity [7], and with more general health co-morbidities such as anxiety, depression, diabetes, cardiovascular disorders, respiratory problems, and gastrointestinal diseases. [8, 9] Some spinal disorders, such as osteopenia, osteomalacia, and tuberculosis, are affected by factors such as nutrition, living conditions and other psychosocial elements. These disorders are related to comorbidities that are also systemic, such as endocrine disorders and infection. Coexistence of two or more conditions, especially over a long period of time, have been associated with lower quality of life, poorer functional status, and increased utilization of health care. [8]
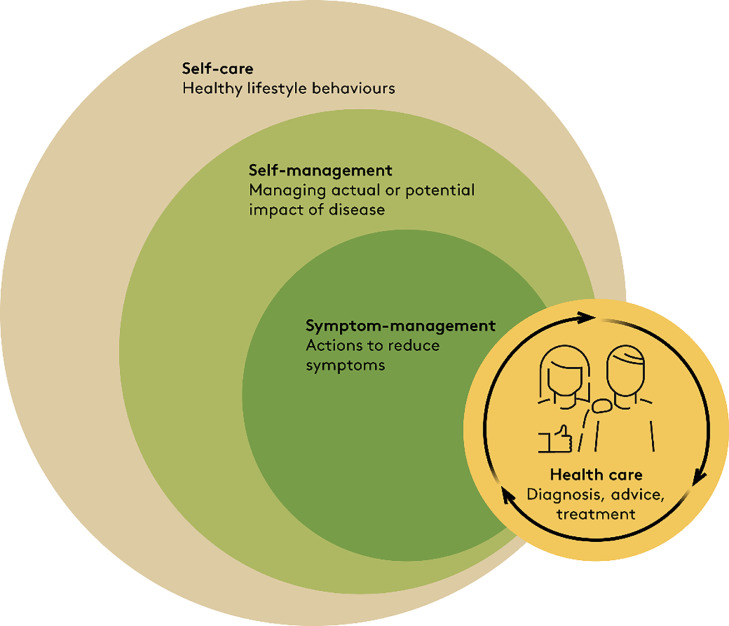
World Spine Care (WSC, www.worldspinecare.org) was established in 2008 with the mission, “to improve lives in underserved communities through sustainable, integrated, evidence-based spinal care.” The WSC vision is to promote, “a world in which everyone has access to the highest quality spine care possible.” The Global Spine Care Initiative (GSCI) is a research proposal created by WSC to reduce the global burden of disease and disability by bringing together leading health care scientists and specialists, government agencies, and other stakeholders to transform the delivery of spine care in underserved and low-income communities worldwide. One of the goals of the GSCI is to provide an evidence-based care pathway and model of care to guide clinicians, policy makers, and public health programs toward a reduction in the burden of spinal disorders. Thus, to understand the general scope of risk factors for commonly presenting spinal disorders, we volunteered to perform a scoping review of this topic so that prevention measures could be considered in a spine care pathway.
While reviews of risk factors, prognostic factors, and comorbidities have been published for individual spinal disorders, we are unaware of any reviews that have cataloged these variables for a range of common spinal disorders. The purpose of this scoping review was to identify risk factors, prognostic factors, and comorbidities associated with the most common spinal disorders that contribute to the greatest burden on society and are likely to be seen by most health care providers globally.
Read the rest of this Full Text article now!



Leave A Comment