Contemporary Biopsychosocial Exercise Prescription for Chronic Low Back Pain:
Questioning Core Stability Programs and Considering Context
SOURCE: J Can Chiropr Assoc. 2017 (Mar); 61 (1): 6–17
Peter Stilwell, B Kin, DC, MSc and Katherine Harman, PT, PhD
Dalhousie University,
5869 University Ave.
PO Box 15000
Halifax, NS B3H 4R2

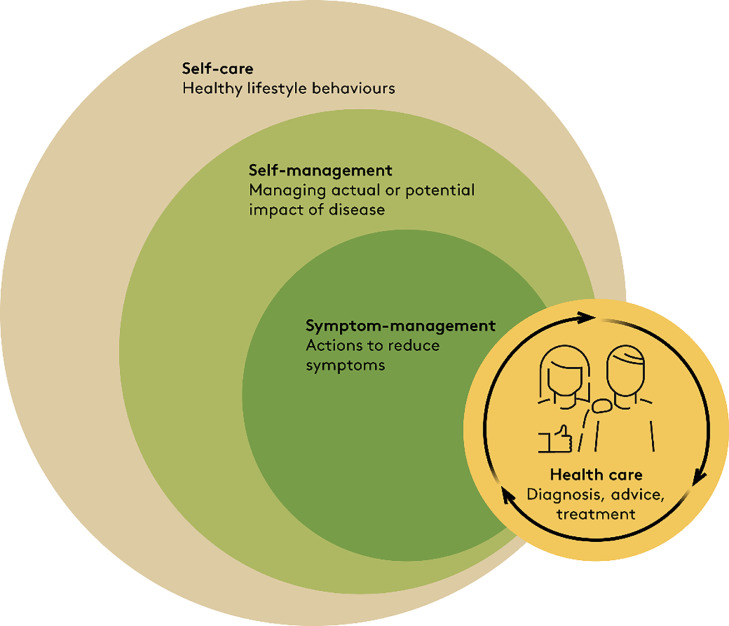
This commentary explores the importance of considering the biopsychosocial model and contextual factors when prescribing exercise. Diverse exercise programs for patients with chronic low back pain (CLBP) produce similar outcomes, without one specific exercise protocol demonstrating clear superiority. One clear barrier to positive outcomes is poor exercise adherence. We suggest that there are certain common contextual factors present in all exercise prescription scenarios that may impact adherence and health-related outcomes. While challenging common core stability exercise prescription, we present an argument for enhancing and intentionally shaping the following contextual factors: the therapeutic alliance, patient education, expectations and attributions of therapeutic success or failure, and mastery or cognitive control over a problem. Overall, this commentary argues that to improve exercise adherence and outcomes in the CLBP population, the context in which exercise is delivered and the meaning patients embody need to be considered and shaped by clinicians.
KEYWORDS: chiropractic; chronic; exercise; low back pain; prescription
From the FULL TEXT Article:
Burden of low back pain
Low back pain (LBP) is the leading cause of disability worldwide. [1] Many individuals with a LBP episode will not be pain-free within a year, despite seeking care from a general practitioner or chiropractor. [2] Although many individuals with acute LBP (pain for less than three weeks) see improvements over time; up to 73% will have a recurrence within 12 months. [3]
There are more articles like this @ our:
Individuals with chronic low back pain (CLBP; pain for greater than three months) also have poor outcomes; 60–80% of those seeking help will continue to have LBP after one year. [4] Data shows that disability from back pain has increased since the late 1990’s, despite advances in technology, improved imaging techniques, and a plethora of available passive interventions. [5] In light of this high burden, it is worthwhile to examine the effectiveness of CLBP treatments; including frequently prescribed exercise programs.
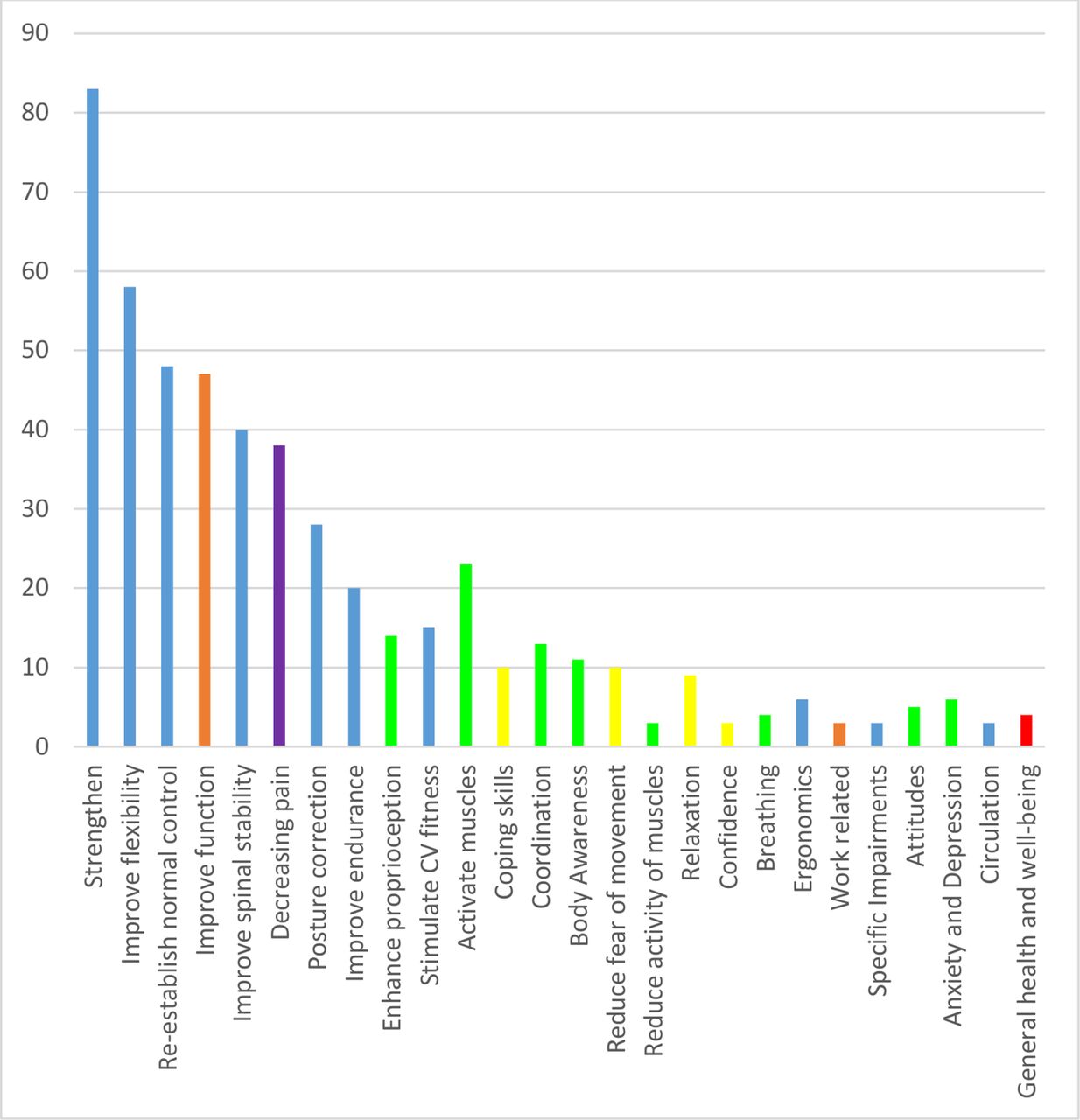
Prescribing exercise for CLBP
Exercise is one of the few interventions for CLBP that has consistently been demonstrated to reduce pain and improve function. [6] Exercise alone or in combination with education is also an effective LBP prevention strategy. [7] Although effect sizes for exercise are modest in reducing pain and improving function [8, 9] it is a desirable part of a treatment program because it is a safe self-management technique that can be performed outside of the clinical environment. As a result, it is possibly the most cost-effective and evidence-informed intervention currently available for CLBP. Unfortunately, while exercise can be effective, only a small percentage of patients with CLBP adhere to a prescribed exercise program, and poor adherence is associated with poor outcomes. [10, 11] In other words, patients have to do the exercise to reap the benefit. While there are many potential barriers to exercise adherence in patients with CLBP, diagnostic uncertainty and fear of pain or harm are among the most commonly cited. [12]
Read the rest of this Full Text article now!




Leave A Comment