Sustained Improvement of Heart Rate Variability in Patients Undergoing a Program of Chiropractic Care: A Retrospective Case Series
SOURCE: Chiropractic Journal of Australia 2018; 45 (4): 338–358 ~ FULL TEXT
Amy Louise Haas, PhD, DC, David Russell, BSc (Psych), BSc (Chiro), Cert TT
Private Practice,
Nashua, NH, USA
Objective: The purpose of this study was to report the sustained changes in heart rate variability (HRV) observed in 6 patients undergoing continuous chiropractic care for the correction of vertebral subluxations.
Clinical Features: Six patients between 25 to 55 years of age all presented with primarily musculoskeletal complaints for chiropractic care in a private practice setting. All patients were nonsmokers with no reported cardiac pathology. All patients were initially assessed for indicators of vertebral subluxation before being accepted for chiropractic care, and were monitored for changes in HRV scores over time.
Intervention and Outcomes: Chiropractic care, using Diversified and Thompson techniques to correct vertebral subluxations, was provided for an initial period of 10 to 52 weeks at a frequency of 2 to 3 visits per week. HRV, measured by SSDN, increased over the early part of their course of chiropractic care, and these increases were sustained whilst the patient remained under long term continuous care in all 6 patients. Improvements in SDNN ranged from 50% to greater than 300% as compared to pre-care values.
Conclusion: Patients receiving continuous chiropractic care to correct vertebral subluxation demonstrated a sustained improvement in heart rate variability (HRV). This novel finding objectively demonstrates long-term change consistent with improved neurophysiological regulation, adaptability and resilience in patients undergoing chiropractic care, and suggests the utility of chiropractic care for outcomes greater than only musculoskeletal improvements.
Key Indexing Terms: Chiropractic; Heart Rate Variability
From the FULL TEXT Article:
Introduction
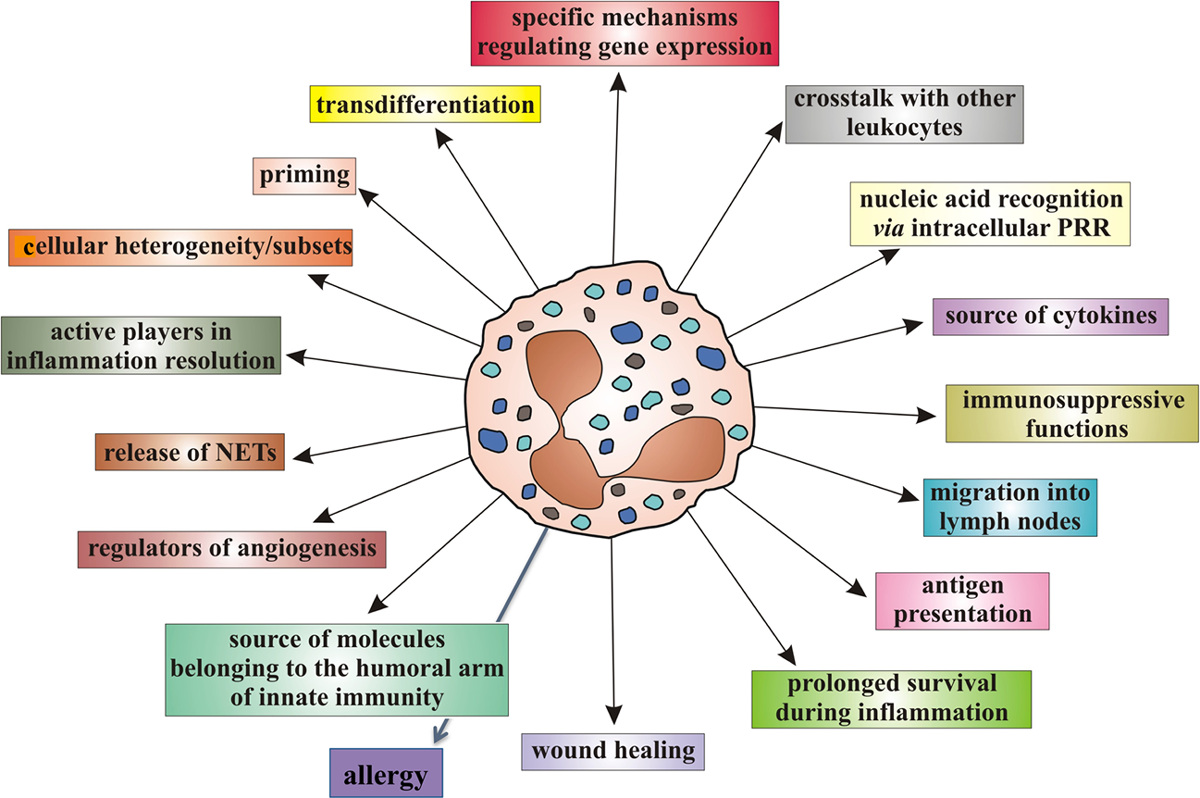
The primary objective of chiropractic care is to optimize health and wellbeing through the enhancement of nervous system function by reducing nerve interference caused by vertebral subluxations. [1–3] The ustralian Spinal Research Foundation defines vertebral subluxation as “a diminished state of being, comprising of a state of reduced coherence, altered biomechanical function, altered neurological function and altered adaptability.” [4] A vertebral subluxation has been recognised as a complex of functional and/or structural changes in the articulations of the spine and pelvis that compromise neural integrity and may influence organ system function and general health. [5] The correction of vertebral subluxations is achieved through chiropractic adjustments that are a typically manually performed. [1, 2, 6] Research over the past 2 decades has shown that the chiropractic adjustment (also referred to as chiropractic spinal manipulation in the chiropractic research literature) results in changes in spinal biomechanics and structure [7–11], central nervous system function [12–16], motor output [17–20], and autonomic output. [21, 22]
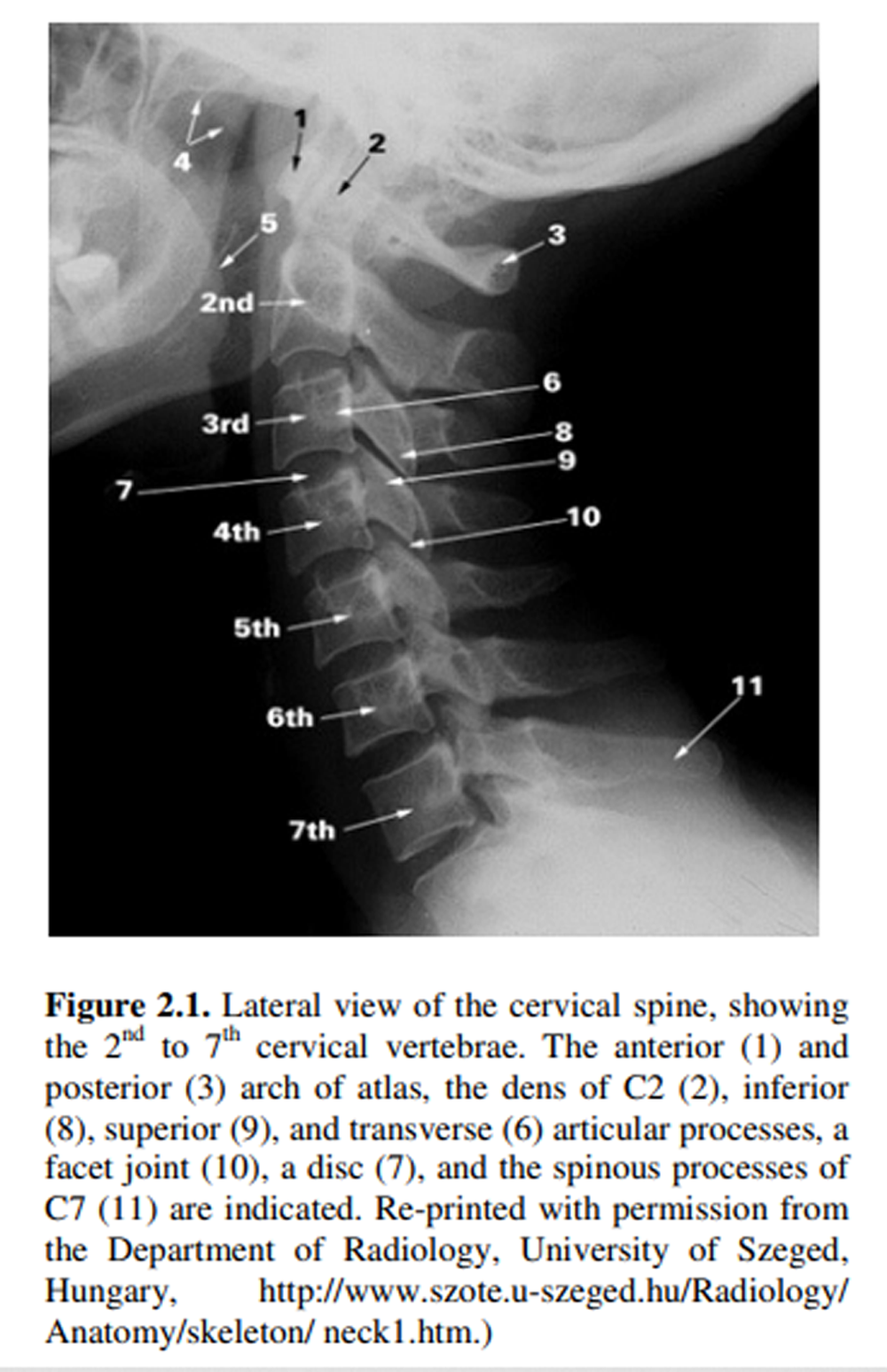
Using objective measures of spinal and neurological function provides the means to quantitatively observe the effects of the chiropractic adjustment. Objective measures used in chiropractic clinical practice to identify the site of intervention and/or to measure outcomes often include both musculoskeletal assessments such as pre- and post-adjustment x-ray, leg length inequality, posture or gait changes, sEMG, algometry, range of motion, motion and static palpation [23], and non-musculoskeletal metrics such as paraspinal thermal balance, heart rate, blood pressure, respiration, reaction time, head repositioning sense, and balance testing. [23, 24] While each measure represents a unique and targeted view on structural and/or physiological changes associated with the chiropractic adjustment, employing alternative outcomes assessment technology allows for the opportunity to expand our understanding of the effects of the adjustment in a way that reflects global changes in autonomic nervous system function and adaptability, and also interfaces with multiple healthcare disciplines. [25]
Measurement of heart rate variability (HRV) has been documented as an effective method to objectively measure improvement in nervous system function. Originally conceived as an assessment tool for cardiac physiology [26], HRV reflects the influence of the Vagus nerve and the sympathetic nervous system on intrinsic heart rhythm [25–27] and therefore HRV monitoring represents a unique window into autonomic nervous system function.
Studies of HRV in the past 2 decades have established that decreased HRV, or “vagal tone”, correlates and/or predicts pathological conditions such as
cardiovascular disease [26–28],
inflammation [29–31],
diabetic neuropathy [32],
emotional dysregulation and post-traumatic stress disorder [33–37],
sleep disorders [38], and
cancer. [38–41]
Read the rest of this Full Text article now!



Leave A Comment