Collaborative Care for a Patient with Complex Low Back Pain and Long-term Tobacco Use: A Case Report
SOURCE: J Can Chiropr Assoc. 2015 (Sep); 59 (3): 216–225
Michael B. Seidman, MSW, DC, Robert D. Vining, DC, Stacie A. Salsbury, PhD, RN
Palmer Center for Chiropractic Research,
Davenport, Iowa.
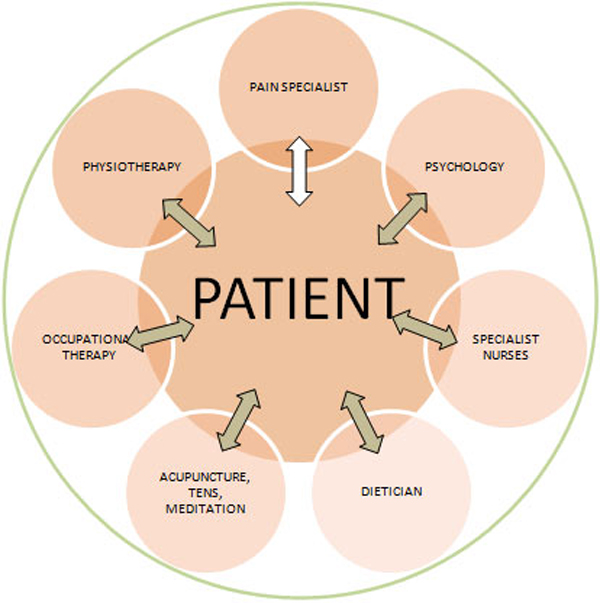
Few examples of interprofessional collaboration by chiropractors and other healthcare professionals are available. This case report describes an older adult with complex low back pain and longstanding tobacco use who received collaborative healthcare while enrolled in a clinical trial. This 65 year-old female retired office worker presented with chronic back pain. Imaging findings included disc extrusion and spinal stenosis. Multiple co-morbidities and the complex nature of this case substantiated the need for multidisciplinary collaboration. A doctor of chiropractic and a doctor of osteopathy provided collaborative care based on patient goal setting and supported by structured interdisciplinary communication, including record sharing and telephone consultations. Chiropractic and medical interventions included spinal manipulation, exercise, tobacco reduction counseling, analgesic use, nicotine replacement, dietary and ergonomic recommendations, and stress reduction strategies. Collaborative care facilitated active involvement of the patient and resulted in decreased radicular symptoms, improvements in activities of daily living, and tobacco use reduction.
There are more articles like this @ our:
Integrated Health Care Page and the:
Keywords chiropractic; integrative medicine; interdisciplinary communication; low back pain; patient-centered care; radiculopathy; spinal manipulation; tobacco use cessation
From the FULL TEXT Article:
Introduction
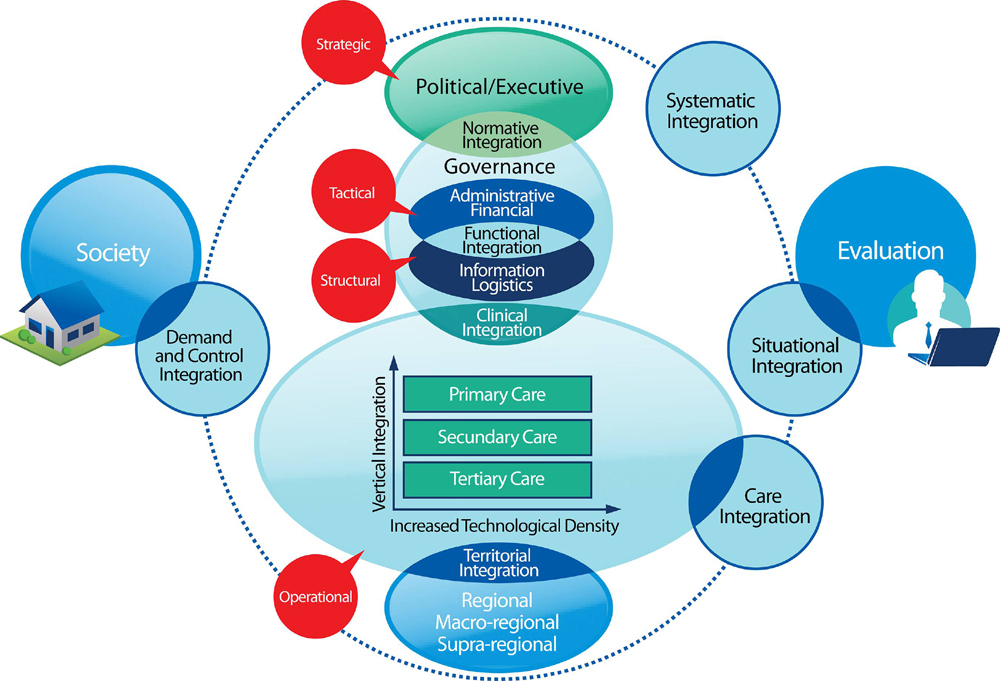
Older adults with low back pain (LBP) often represent a complex clinical picture due to the inherent challenges of treating LBP especially when combined with multiple co-morbidities. [1–4] Given the potential for such complexity, it is important for clinicians and patients to consider these elements as management plans are designed and implemented. [2, 5] Multidisciplinary collaborative care including care coordination among providers is one possible approach to the management of complex LBP. [1, 2, 6, 7]
Boon and colleagues defined collaborative care as “an interprofessional process for communication and decision making that enables the separate and shared knowledge and skills of health providers to synergistically influence patient care.” [8, 9]
Successful collaboration requires
mutual respect [9, 10, 12],
maintenance of professional autonomy [8, 13, 14],
understanding each team members’ practice scope [9, 13, 15–17],
goal setting [9, 10, 13], and
an openness to discussion and consensus building processes. [13]
or face-to-face meetings [10, 16, 18, 21],
job shadowing experiences [9, 16, 20],
use of electronic medical records [9, 14, 18],
and confirming understanding among team members. [12, 19, 21]
Case presentation
Read the rest of this Full Text article now!


Leave A Comment