Report of the NIH Task Force on Research Standards for Chronic Low Back Pain
SOURCE: Int J Ther Massage Bodywork. 2015 (Sep 1); 8 (3): 16–33 ~ FULL TEXT
Richard A. Deyo, MD, MPH, Samuel F. Dworkin, DDS, PhD,
Dagmar Amtmann, PhD, Gunnar Andersson, MD, PhD,
David Borenstein, MD, Eugene Carragee, MD,
John Carrino, MD, MPH, Roger Chou, MD, Karon Cook, PhD,
Anthony DeLitto, PT, PhD, Christine Goertz, DC, PhD,
Partap Khalsa, DC, PhD, John Loeser, MD, Sean Mackey, MD, PhD,
James Panagis, MD, James Rainville, MD, Tor Tosteson, ScD,
Dennis Turk, PhD, Michael Von Korff, ScD, and Debra K. Weiner, MD
Oregon Health and Sciences University,
Portland, OR.
Despite rapidly increasing intervention, functional disability due to chronic low back pain (cLBP) has increased in recent decades. We often cannot identify mechanisms to explain the major negative impact cLBP has on patients’ lives. Such cLBP is often termed non-specific, and may be due to multiple biologic and behavioral etiologies. Researchers use varied inclusion criteria, definitions, baseline assessments, and outcome measures, which impede comparisons and consensus. The NIH Pain Consortium therefore charged a Research Task Force (RTF) to draft standards for research on cLBP. The resulting multidisciplinary panel recommended using 2 questions to define cLBP; classifying cLBP by its impact (defined by pain intensity, pain interference, and physical function); use of a minimal data set to describe research participants (drawing heavily on the PROMIS methodology); reporting “responder analyses” in addition to mean outcome scores; and suggestions for future research and dissemination. The Pain Consortium has approved the recommendations, which investigators should incorporate into NIH grant proposals. The RTF believes these recommendations will advance the field, help to resolve controversies, and facilitate future research addressing the genomic, neurologic, and other mechanistic substrates of chronic low back pain. We expect the RTF recommendations will become a dynamic document, and undergo continual improvement.
KEYWORDS:   NIH Task Force; chronic low back pain; low back pain; minimum dataset; research standards
From the FULL TEXT Article:
Introduction
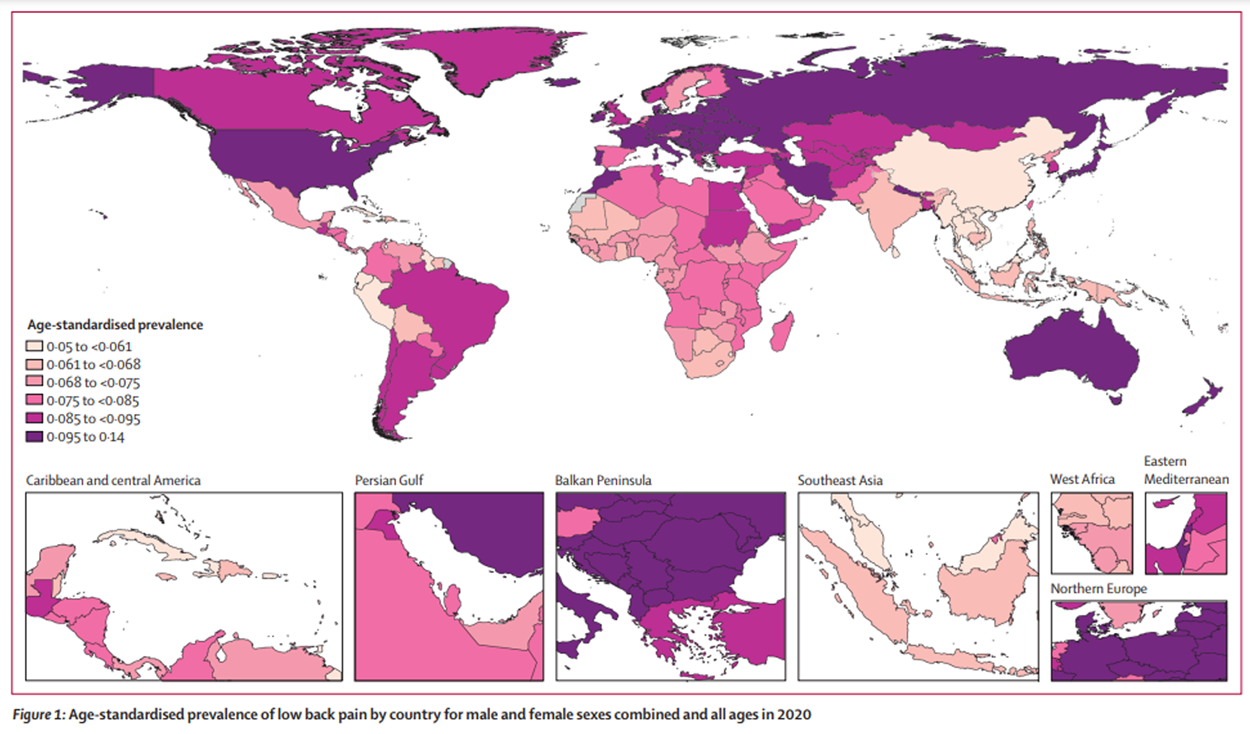
The Institute of Medicine recently estimated that chronic pain affects about 100 million adults in the United States, with an estimated annual cost of $635 billion, including direct medical expenditures and loss of work productivity. [3] Activity-limiting low back pain (LBP), in particular, has a world-wide lifetime prevalence of about 39% and a similar annual prevalence of 38%. [61] The majority of people having LBP experience recurrent episodes. [62] The use of all interventions for treating chronic LBP (cLBP) increased from 1995–2010, including surgery, pharmacological, and non-pharmacological approaches. Despite increased utilization, however, the prevalence of symptoms and expenditures has increased. [37, 70, 91]
There are more articles like this @ our:
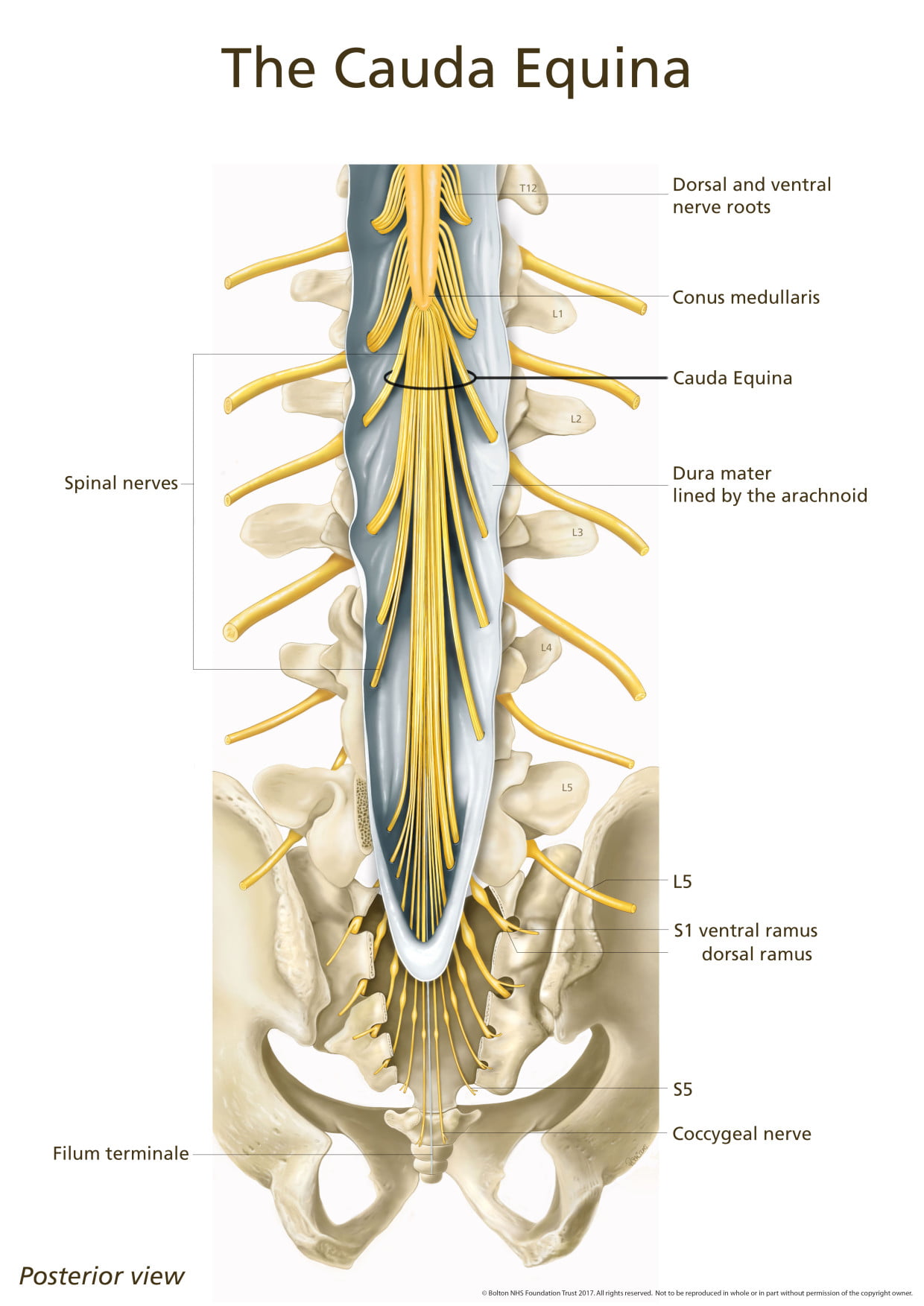
There is growing evidence that cLBP, like other chronic pain conditions, can progress beyond a symptomatic state to a complex condition unto itself, [109] involving persistent anatomical and functional changes in the central nervous system [9, 93, 100] in addition to structural changes in the back (e.g., degenerative spinal changes, atrophy or asymmetry of para-spinal muscles). [10, 11, 14] Although some patients with cLBP may have clear pathoanatomic etiologies, for many there is no clear association between pain and identifiable pathology of the spine or its associated soft tissues. [26]
Many patients who undergo procedures intended to correct the putative causative pathoanatomy continue to have pain. Furthermore, we often cannot identify mechanisms to account for the substantial negative impact cLBP has on the lives of many patients. [20] Such cLBP is often termed non-specific, idiopathic, mechanical, or due to instability, and may in fact be due to the contributions of different and multiple biologic and behavioral etiologies in different individuals. [87]
Read the rest of this Full Text article now!


Leave A Comment