What Happened To The ‘Bio’ In The Bio-psycho-social Model of Low Back Pain?
SOURCE: Eur Spine J. 2011 (Dec); 20 (12): 2105-2110
Mark J. Hancock, Chris G. Maher, Mark Laslett, Elaine Hay, and Bart Koes
Faculty of Health Sciences,
University of Sydney,
PO Box 170,
Lidcombe 1825, NSW, Australia.
mark.hancock@sydney.edu.au
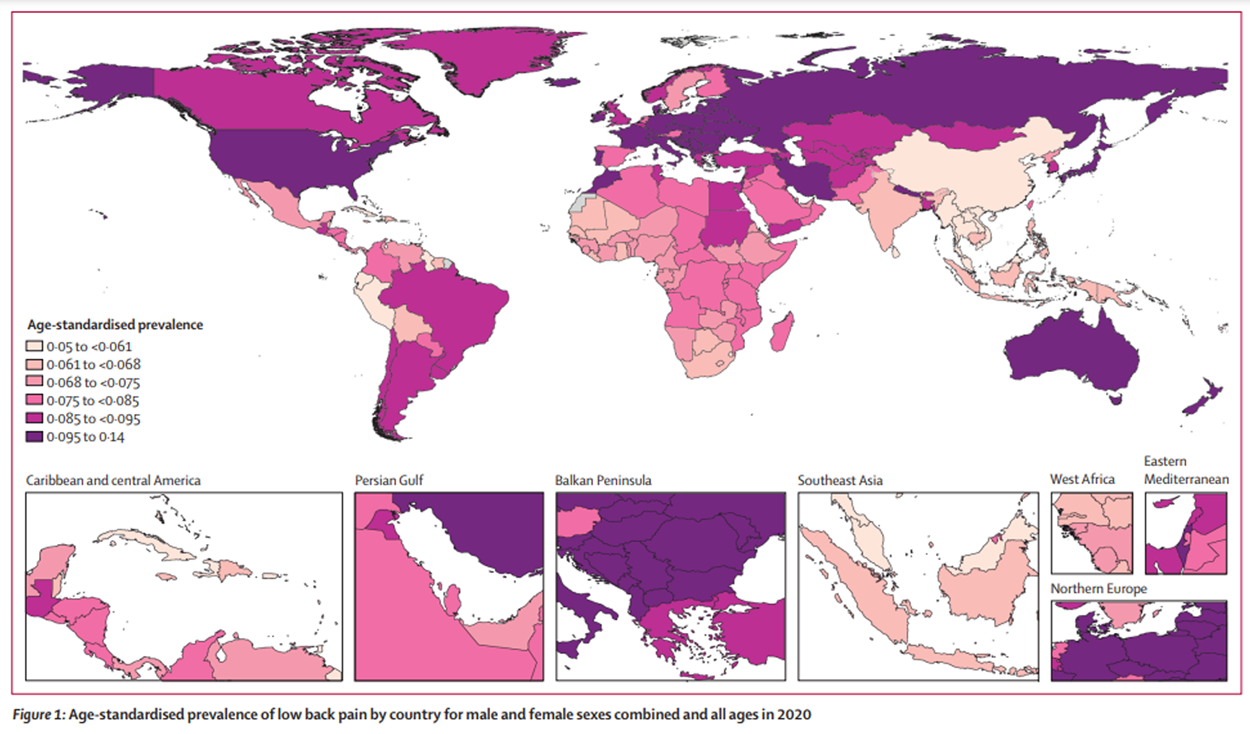
Purpose Over 20 years ago the term non-specific low back pain became popular to convey the limitations of our knowledge of the pathological source of most people’s low back pain. Knowledge of underlying pathology has advanced little since then, despite limited improvements in outcomes for patients with low back pain.
Methods This paper discusses potential misunderstandings related to diagnostic studies in the field of low back pain and argues that future diagnostic studies should include and investigate pathological sources of low back pain.
Results Six potential misunderstandings are discussed.
- Until diagnosis is shown to improve outcomes it is not worth investigating;
- without a gold standard it is not possible to investigate diagnosis of low back pain;
- the presence of pathology in some people without low back pain means it is not important;
- dismissal of the ability to diagnose low back pain in clinical guidelines is supported by the same level of evidence as recommendations for therapy;
- suggesting use of a diagnostic test in research is misinterpreted as endorsing its use in current clinical practice;
- we seem to have forgotten the ‘bio’ in biopsychosocial low back pain.
Conclusions We believe the misunderstandings presented in this paper partly explain the lack of investigation into pathology as an important component of the low back pain experience. A better understanding of the biological component of low back pain in relation, and in addition, to psychosocial factors is important for a more rational approach to management of low back pain.
Keywords: Low back pain, Diagnosis, Back pain
There are more articles like this @ our:
From the FULL TEXT Article
Introduction
Over the last three decades there has been a major shift in the clinical and research approach to low back pain. Prior to this, clinical practice and research activities were mainly based upon a biomedical model with patients receiving specific pathoanatomical diagnoses and treatments directed to these diagnoses. A notable example of this type of thinking is Mixter and Barr’s 1934 classic paper describing surgical treatment of disc prolapse [1]. This traditional approach was challenged in 1987 by two landmark publications that correctly pointed out that most diagnoses were nominal and of doubtful validity. Gordon Waddell’s seminal paper titled “A new clinical model for the treatment of low-back pain” [2] introduced the biopsychosocial model of low back pain, emphasizing the distinction between pain and disability and the need to address the biological, psychological and social aspects of the condition. He promoted the term “simple back pain” to describe the majority of patients with this common symptom in whom a specific source of pain could not legitimately be identified. The report of the Quebec task force [3] used the term “nonspecific spinal disorder” to describe the same patients. Importantly while both documents highlighted the problems with existing diagnostic tests they also identified the need for future research to identify methods and tests that would allow clinicians to determine the source of a patient’s pain. [2, 3]
Read the rest of this Full Text article now!


Leave A Comment