The Collateral Benefits Of Having Chiropractic Available In A Public Central Hospital
Journal of Hospital Administration 2013 (Aug 8); 2 (4): 138–143 ~ FULL TEXT
Jan Roar Orlin, Andrè Didriksen, Helge Hagen, Anders Sørfonden
Dept. of Orthopedics, Central Hospital (FSS), Førde, Norway, and
Dept. of Ear-Nose-Throat, Central Hospital (FSS), Førde, Norway
Thanks to Dana Lawrence, DC for drawing our attention to this article!
Following previous reports on the co-operation between a chiropractor and a central hospital, experiences from the past five years are presented. The objective of this paper is to show that improved management of muscular and skeletal problems within a hospital setting depends on the availability of chiropractic health care as a treatment option.
The following pain groups were sampled:
1) sacro-lumbar dysfunction and sciatic leg symptoms, with or without joint dysfunction and sciatica;
2) myo-fascial referred pain syndromes, frequently caused by peripheral nerve entrapment; and
3) tinnitus, dizziness/vertigo, facial pain, ear plug and swallowing difficulties, frequently caused by biomechanical components.
A majority of pain patients, after being subjected to traditional conservative treatment, usually over a period of several years, fail to return to work despite younger than average age. The only effective procedures seem to be those of chiropractors. In order to benefit from their particular knowledge, public hospitals need to open their doors to chiropractors. For that to happen, determined hospital administrators are needed.
1. Introduction
Patients with muscular and skeletal problems may become a burden to National Health budgets. In public hospitals, highly-specialized teams offer evidence-based medicine and modern diagnostic procedures and treatments to patients with widespread muscle pain. Many specialties are involved. Yet, the national costs of muscular and skeletal pain seem unaffected by these interventions, and are steadily increasing. Pain clinics, composed of multiple specialty groups, were instituted to offer solutions to patients incapacitated by all kinds of muscular and skeletal pain, but in practice they frequently do not meet expectations. In this setting, orthopedic surgeons have become extremely sub-specialized, often treating degenerative joint disease and fractures in only one part of the body, whereas chiropractors treat functional lesions in the entire body. Unfortunately, the interest of the medical profession in understanding chiropractic principles has not been high.
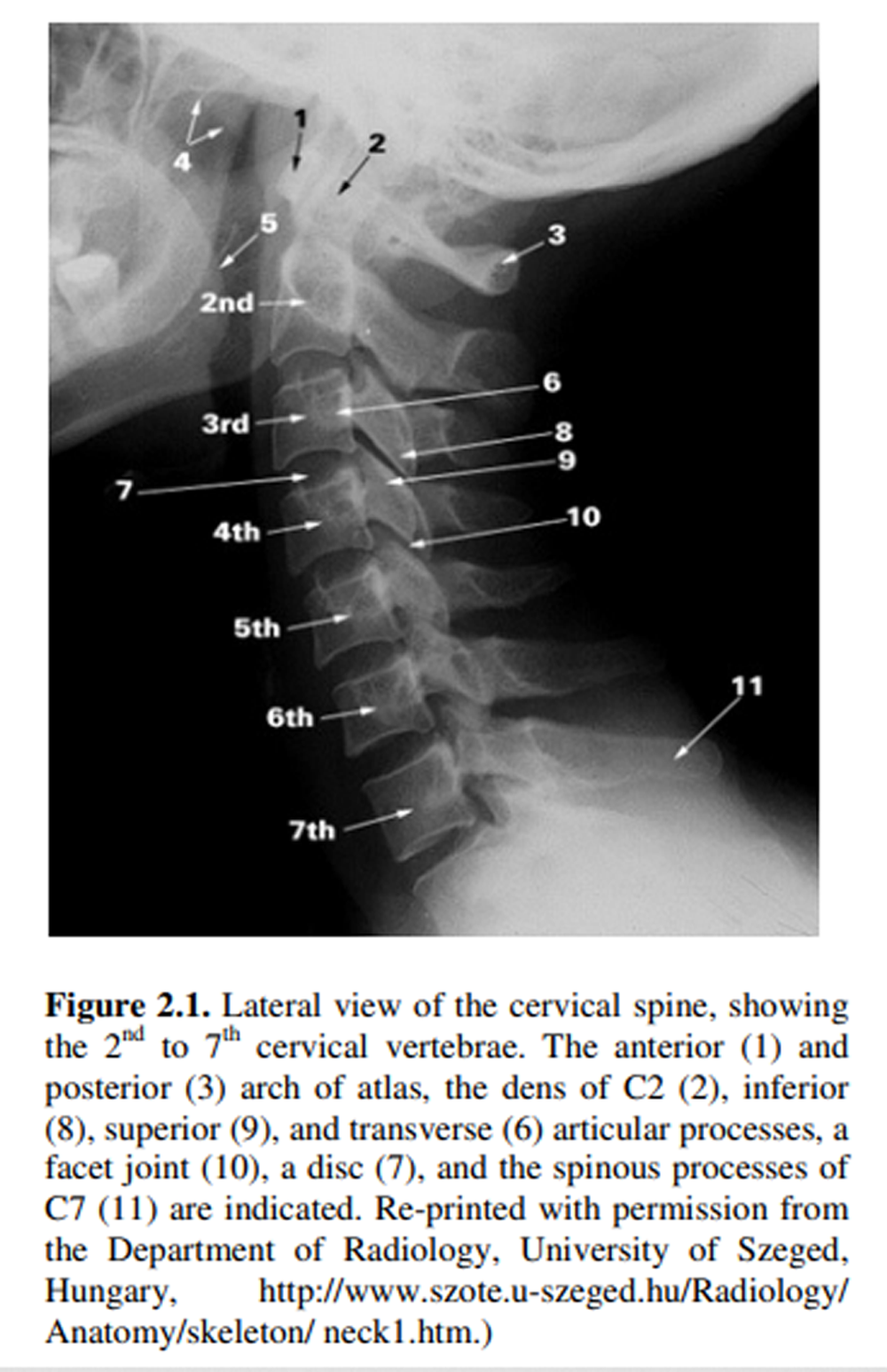
Traditionally, hospital medical staffs have considered the treatment offered by chiropractors to be of dubious value and not grounded on evidence-based research. However, chiropractic care now has a growing body of evidence-based research. [1] Leading chiropractic teaching institutions in the world have science-based educational programs comparable to those of medical teaching institutions. Research by Triano in 1992 led to definition of the basic concept of a functional spinal lesion. [2] When the interaction between the nervous system, facet joints with their movement receptors and the musculature is disturbed, a functional spinal lesion follows. A neuro-biomechanical approach to restore normal balance created by monosynaptic reflexes acting between joints and the deep spinal muscles is needed. With patients placed in a prone or supine position to relax them, soft tissue techniques, aimed at affecting muscle tone at the site of primary joint lesions and at secondary compensatory lesions, are used. These techniques include pressure on local muscular pain locations (= trigger points), often in combination with passive stretching and traction to achieve relaxation. The main treatment consists of joint adjustment techniques which is a fast passive stretching of deep structures around the joint, with the utmost importance placed on appropriate force, speed, amplitude and movement specificity.
In a few universities in some countries, medical and chiropractic students spend their first years under the same roof. The result has not only been mutual acknowledgement, but also a new and exciting combination of medical doctor and chiropractor. In recognition of chiropractors’ ability to reduce muscular-skeletal pain and increase function, Norwegian chiropractors in 2006 were given the right to report patients sick and to refer them to specialists. Otherwise, the possible advantages of muscular and skeletal pain reduction and cost benefits from closer cooperation between chiropractors and hospital staffs have been given few incentives. In Norway, two areas may contribute to improvements: emerging plans to start educating chiropractors at one of the universities and large-scale research into diseases causing muscular and skeletal pain, with financing, initiated by the Norwegian Department of Health. [3]
Read the rest of this Full Text article now!



Why the disdain for chiropractic? The science has millions of contented patients and it has been proven as a reliable treatment for not only back pain but other conditions as well. The medical community needs to remove their bias and actually read the research!