Cerebral Perfusion in Patients with Chronic Neck and Upper Back Pain: Preliminary Observations
SOURCE: J Manipulative Physiol Ther. 2012 (Feb); 35 (2): 76-85
Maxim A. Bakhtadze, MD, PhD, Howard Vernon, DC, PhD, Anatoliy V. Karalkin, MD, PhD, Sergey P. Pasha, MD, PhD, Igor O. Tomashevskiy, MD, PhD, David Soave, MS
Center for Manual Therapy, Moscow, Russia.
OBJECTIVE: The purpose of this study was to determine the correlation between cerebral perfusion levels, Neck Disability Index (NDI) scores, and spinal joint fixations in patients with neck pain.
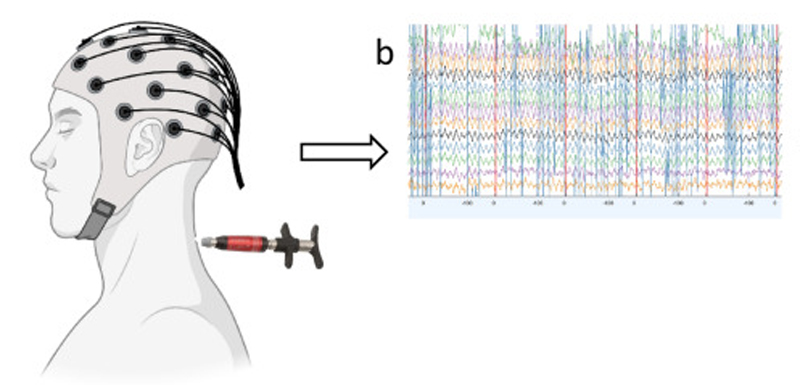
METHODS: Forty-five adult patients (29 were female) with chronic neck/upper thoracic pain during exacerbation were studied. The subjects were grouped according to NDI scores: mild, moderate, and severe. The number of painful/blocked segments in the cervical and upper thoracic spine and costovertebral joints, pain intensity using the visual analog scale, and regional cerebral blood flow of the brain using single-photon emission computed tomography (SPECT) were obtained. The SPECT was analyzed semi-quantitatively. Analysis of variance tests were conducted on total SPECT scores in each of the NDI groups (P < .05). Univariate correlations were obtained between blockage, pain, and SPECT scores, as well as age and duration. A multivariate analysis was then conducted.
RESULTS: Group 1 (mild) consisted of 14 patients. Cerebral perfusion measured by SPECT was normal in all 8 brain regions.
Group 2 (moderate) consisted of 16 patients. In this group, a decrease in cerebral perfusion was observed (range, 20%-35%), predominantly in the parietal and frontal zones.
Group 3 (severe) consisted of 15 patients. In this group, the decrease in cerebral perfusion observed was from 30% to 45%, again predominantly in the parietal and frontal zones.
A significant difference was found between NDI groups (“moderate” and “severe” showed significantly greater hypoperfusion than “mild”). Total blockage score correlated with SPECT scores at r = 0.47, P = .001. In a multivariate analysis, NDI scores contributed 39% of the variance of SPECT scores.
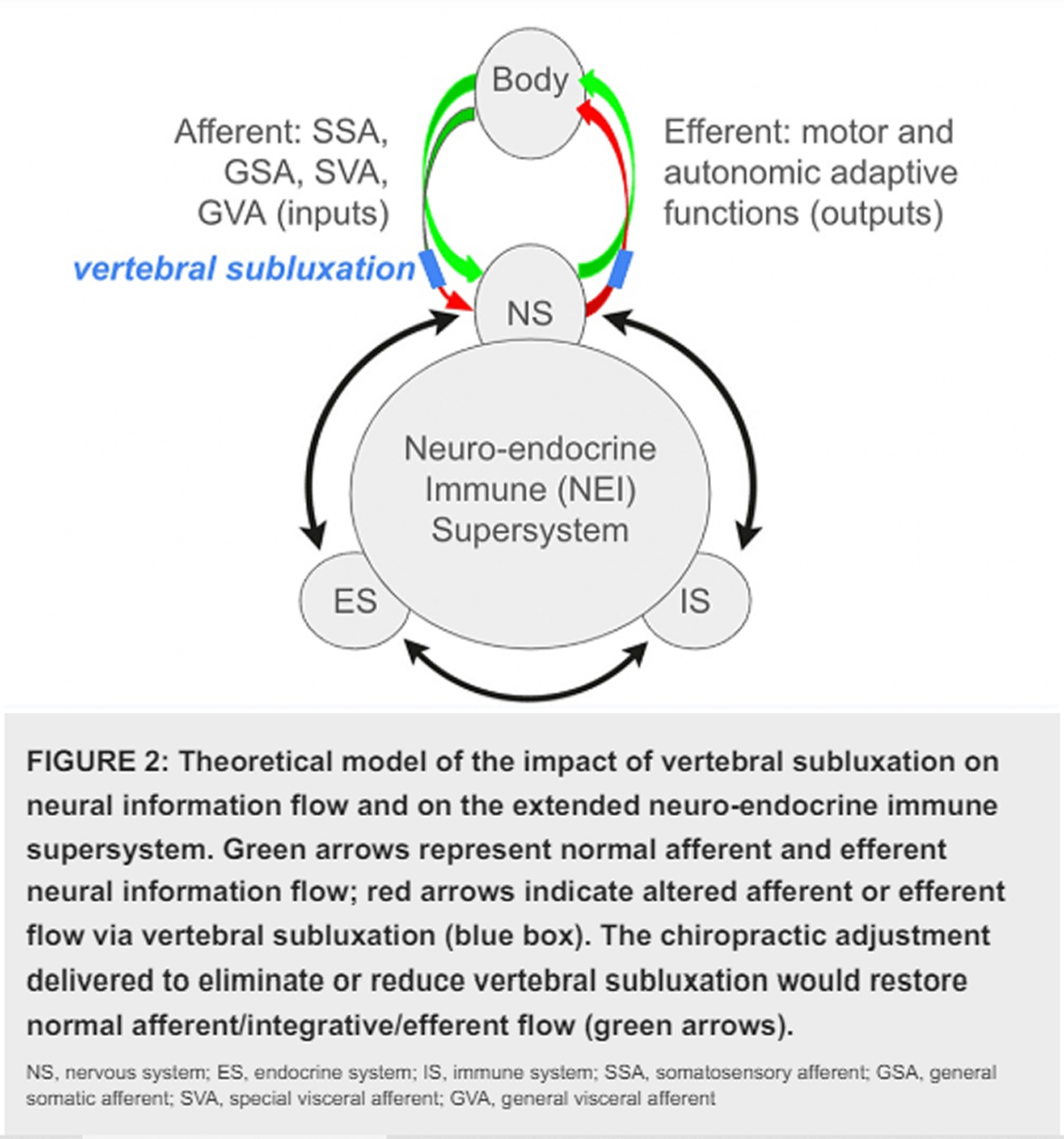
CONCLUSION: In this group of patients with neck and/or upper back pain, NDI scores strongly predicted cerebral hypoperfusion. Spinal joint dysfunction may be involved via hyperactivity in the regional sympathetic nervous system.
From the Full-Text Article:
Discussion
The primary goal of this study was to determine if categorizing patients with chronic neck pain by their NDI scores could distinguish those with and without cerebral perfusion abnormalities, thereby improving the efficiency of using SPECT for this purpose. Our findings strongly support this result. Single-photon emission computed tomography scores in NDI groups 2 and 3 were significantly higher than in group 1. Neck Disability Index scores strongly correlated with SPECT scores, and NDI scores were the only variable loading onto SPECT scores, contributing 39% of the variance of those scores.
Our findings replicate the strong correlation between NDI and PET scores reported by Linnman et al, [28] with their finding of temporo-occipital hypoperfusion in patients with WAD. This correlation between disability level and perfusion status may explain some of the inconsistencies in the previous studies of SPECT in neck pain. [23-31] According to our finding, it is the severity of self-reported disability that appears to be associated with cerebral perfusion abnormalities, not the simpler status of WAD vs non-WAD.
The location of reduced rCBF findings in our study—parietal and frontal lobes in groups 2 and 3 — is not in accord with those reported for non-WAD cases by Sundstrom et al [30] and Guez [31]; that is, hypoperfusion in the right temporal region. Our findings are somewhat more similar to those reported by Otte et al [23-26] for patients with WAD—parieto-occipital hypoperfusion. However, technical and methodological issues (see “Limitations” below) make comparisons between these studies difficult.
An explanation for the association between NDI and SPECT scores requires discussion of at least 3 separate domains. First, there is now strong evidence that chronic pain itself is associated with changes in the brain. [46-49] Although we did find that pain level does correlate with SPECT scores, our finding that it is the severity of self-reported disability that statistically distinguishes those with and without such changes is a novel finding, at least for patients with neck pain.

Thanks for explaining this detailed post. Which it will be a big help and makes a big differences to the readers.