Utilization, Cost, and Effects of Chiropractic Care on Medicare Program Costs
An older study of Medicare cost data completed in June (2001 or 2002) by the well-known Washington, DC-based firm Muse & Associates helps demonstrate the cost-saving impact that chiropractic care has on the current Federal Medicare program.
The study, titled “Utilization, Costs, and Effects of Chiropractic Care on Medicare Program Costs“, was commissioned by the ACA and is the first study of its type to compare the global, per capita Medicare expenditures of chiropractic patients to those of non-chiropractic patients receiving care in the federal Medicare program. The study utilizes data obtained from Medicare’s Standard Analytical Files for 1999 — the most recent year that cost data was available for analysis.
The study’s executive summary states:
“The results strongly suggest that chiropractic care significantly reduces per beneficiary costs to the Medicare program. The results also suggest that Chiropractic services could play a role in reducing costs of Medicare reform and/or a new prescription drug benefit.”
The study specifically found that:
- Beneficiaries who received chiropractic care had lower average Medicare payments for all Medicare services than those who did not ($4,426 vs. $8,103);
- Beneficiaries who received chiropractic care averaged fewer Medicare claims per capita than those who did not; and
- Beneficiaries who received chiropractic care had lower average Medicare payments per claim than those who did not.
According to ACA officials, the positive results of the study will be used to bolster ACA’s legislative efforts to expand the availability of chiropractic care in Medicare and to expand the list of chiropractic-related services the Medicare program would reimburse.
A summary of the report prepared by Muse and Associates for the American Chiropractic Association
The report found significant differences in the utilization of services and Medicare payment for beneficiaries who saw doctors of chiropractic versus those who did not. The report has not been finalized, so detailed information is not available yet. The report must go through a long approval process, including the Centers for Medicare and Medicaid Services’ (CMS), formerly known as the Health Care Financing Administration, review of the data. As soon as the Muse report is final, the ACA will make it available.
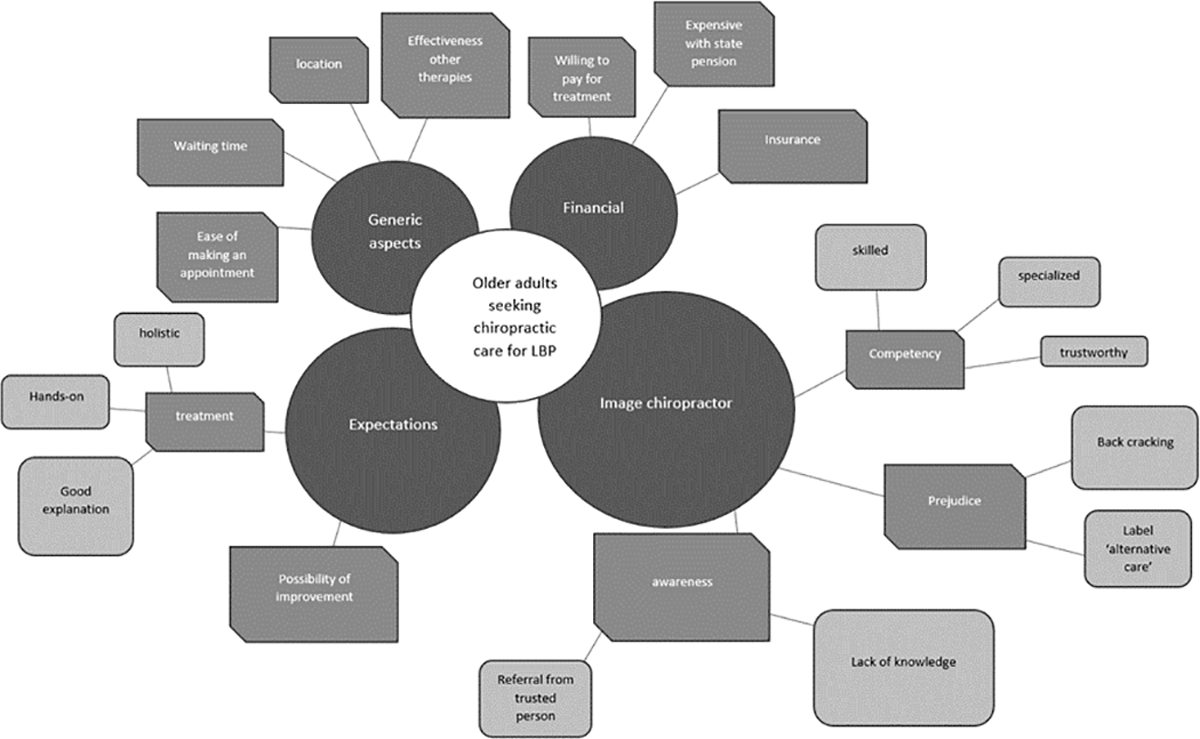
The report utilized data compiled by the CMS, and focuses on Medicare beneficiaries with primary diagnoses of selected musculoskeletal, dislocations, sprains and strains of joints and adjacent muscle conditions. The data, derived from CMS’ 1999 figures, indicates that approximately 5.8 million beneficiaries had a Medicare claim with a principal diagnosis of at least one of the selected medical conditions listed above. Of these individuals, about 1.5 million (26.8 percent) received chiropractic care and 4.3 million (73.2 percent) were treated by other types of providers.
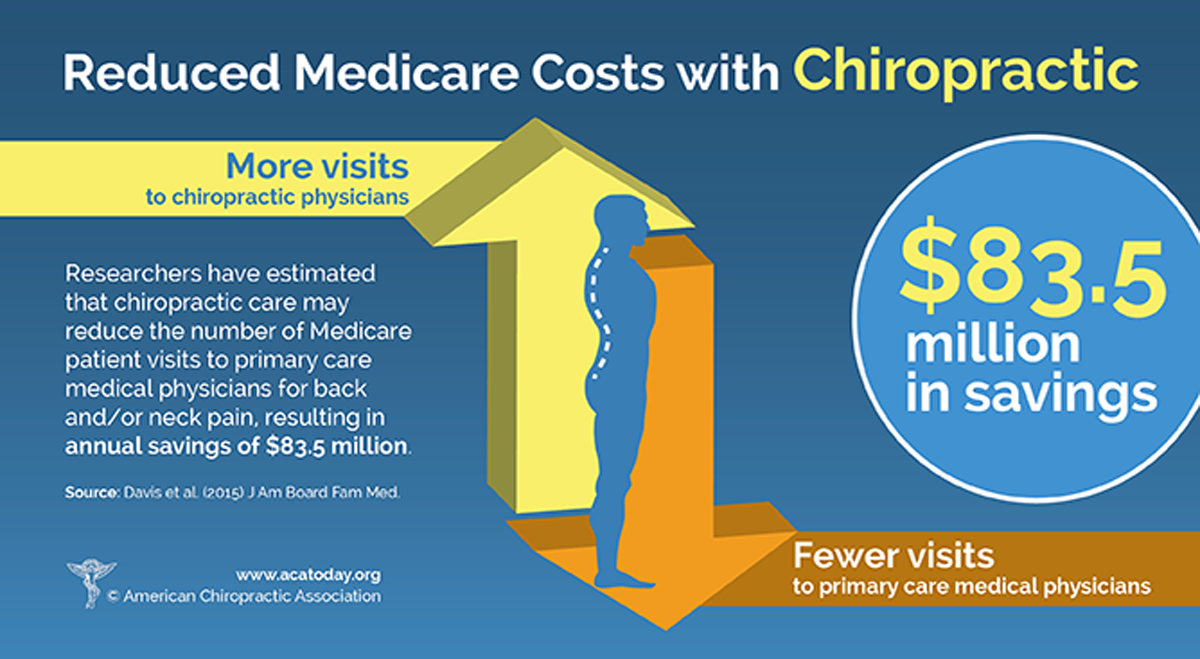
The report’s conclusion suggests that decreased access to chiropractic services would increase the Medicare program’s costs. In addition, the report found that, overall, beneficiaries who used chiropractic services had lower medical doctor costs. Due to these cost savings, the report suggests that during any congressional debate on Medicare reform, consideration should be given to providing increased access to chiropractic care. In addition, the study suggests that some savings would probably accrue in the Medicare program if access to chiropractic services were increased in concert with a Medicare prescription drug benefit.


http://www.medscape.com/viewarticle/746813?src=mp&spon=34
frank, when you have the time please read this review on “spinal manipulation and cervocogenic headaches”.it’s somewhat difficult for me to say there is not a bias in this article. i’m curious about your opinion. thanks
Hi Karl
Not to be funny, but ex-professor Ernst gives me a headache…hehehe
I don’t have the time to de-bone and fillet this thoroughly right now, but it seems the professor is a very harsh critic, bolstered by his extremely limited definitions for and evaluations of research design, terminology and methods, leading to nasty little evaluations like: “This trial lacks allocation concealment, appropriate randomization, and blinding procedures. We scored this study as 2.” in response to Nilsson’s “The Effect of Spinal Manipulation in the Treatment of Cervicogenic Headache”
We really need a qualified researcher to get down into the dirt with these “reviewers” to review their choices, and how that may have led to discounting the power of the studies under review, and to point out studies they may have ignored for one reason or another.
Ernst has taken significant criticism previously for narrow interpretation of research terms and methods, in what appeared to be hatchet jobs on otherwise competent trials, for who-knows what reasons.