Consensus on the Clinical Diagnosis of Lumbar Spinal Stenosis
Consensus on the Clinical Diagnosis of Lumbar Spinal Stenosis: Results of an International Delphi Study
SOURCE: Spine (Phila Pa 1976). 2016 (Aug 1); 41 (15): 1239–1246
Christy Tomkins-Lane, PhD, Markus Melloh, MD, PhD, Jon Lurie, MD, et. al.
Department of Health and Physical Education,
Mount Royal University,
Calgary, Canada
STUDY DESIGN: Delphi.
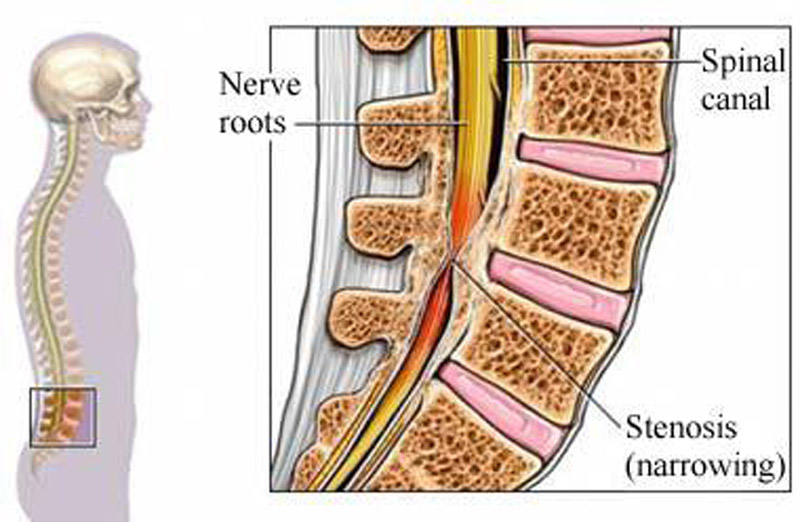
OBJECTIVE: The aim of this study was to obtain an expert consensus on which history factors are most important in the clinical diagnosis of lumbar spinal stenosis (LSS).
SUMMARY OF BACKGROUND DATA: LSS is a poorly defined clinical syndrome. Criteria for defining LSS are needed and should be informed by the experience of expert clinicians.
METHODS: Phase 1 (Delphi Items): 20 members of the International Taskforce on the Diagnosis and Management of LSS confirmed a list of 14 history items. An online survey was developed that permits specialists to express the logical order in which they consider the items, and the level of certainty ascertained from the questions. Phase 2 (Delphi Study) Round 1: Survey distributed to members of the International Society for the Study of the Lumbar Spine. Round 2: Meeting of 9 members of Taskforce where consensus was reached on a final list of 10 items. Round 3: Final survey was distributed internationally. Phase 3: Final Taskforce consensus meeting.
RESULTS: A total of 279 clinicians from 29 different countries, with a mean of 19 (±SD: 12) years in practice participated.
The six top items were
“flex forward to relieve symptoms,”
“feel relief when using a shopping cart or bicycle,”
“motor or sensory disturbance while walking,”
“normal and symmetric foot pulses,”
“lower extremity weakness,” and
“low back pain.”
There are more articles like this @ our:
Low Back Pain and Chiropractic Page
and the: