Proprioceptive Cervicogenic Dizziness: A Narrative Review of Pathogenesis, Diagnosis, and Treatment
SOURCE: J Clinical Medicine 2022 (Oct 26); 11 (21): 6293
Yongchao Li • Liang Yang • Chen Dai • Baogan Peng
The Third Medical Centre of Chinese PLA General Hospital,
Department of Orthopedics,
69 Yongding Road,
Beijing 100039, China.
FROM: J Orthop Sports Phys Ther 2009
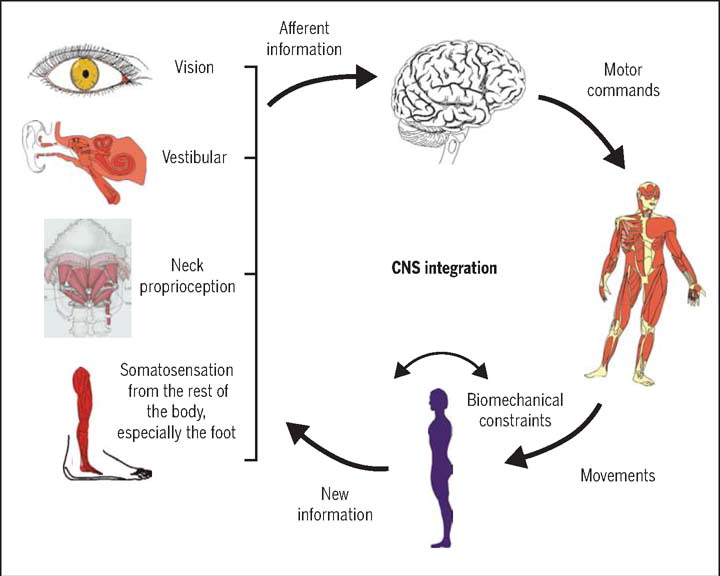
Basic science and clinical evidence suggest that cervical spine disorders can lead to dizziness. The cervical spine has highly developed proprioceptive receptors, whose input information is integrated with the visual and vestibular systems in the central nervous system, acting on the neck and eye muscleThere are many more studiess to maintain the coordinative motion of the head, eyes, neck, and body through various reflex activities.
When the cervical proprioceptive input changes due to the mismatch or conflict between vestibular, visual, and proprioceptive inputs, cervicogenic dizziness may occur. The diagnosis of cervicogenic dizziness can be determined based on clinical features, diagnostic tests, and the exclusion of other possible sources of dizziness. The cervical torsion test appears to be the best diagnostic method for cervicogenic dizziness.
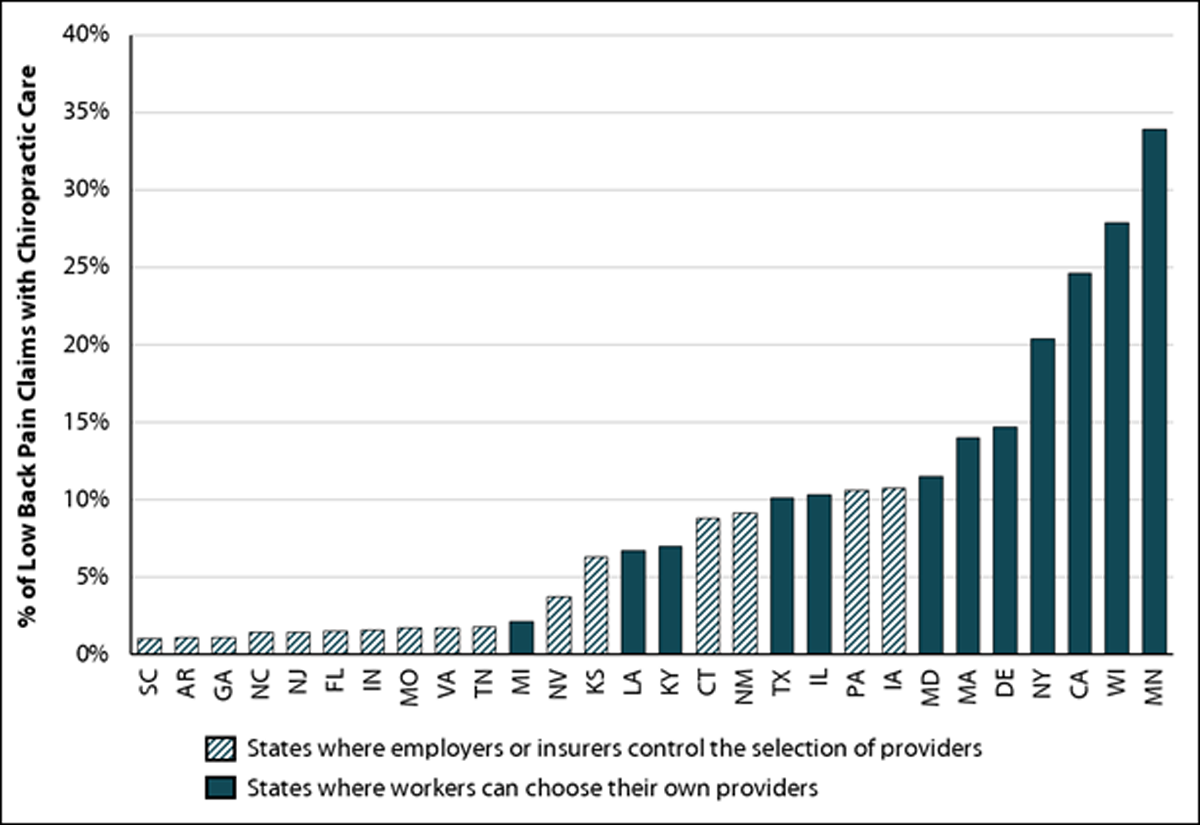
Based on the available evidence, we first developed the diagnostic criteria for cervicogenic dizziness. Treatment for cervicogenic dizziness is similar to that for neck pain, and manual therapy is most widely recommended.
Keywords: cervical proprioception; cervicogenic dizziness; diagnosis; management; neck pain; proprioceptors.
From the FULL TEXT Article:
Introduction
Dizziness is one of the most common reasons for consultation in adult patients. [1, 2] It is an umbrella term used to describe various sensations, including vertigo, disequilibrium, lightheadedness, or presyncope (Table 1). [2] From this perspective, vertigo is just one part of dizziness. However, in the light of the International Bárány Society for NeuroOtology [3], dizziness and vertigo are no longer subordinate but independent allelic symptoms. Dizziness and vertigo may coexist or occur sequentially (Table 2). [3] In 1955, Ryan and Cope [4] first described dizziness caused by neck disorders as cervical vertigo, also known as cervicogenic vertigo, cervicogenic dizziness or cervical dizziness. In this review, we use cervicogenic dizziness to name this trouble. A recent clinical observation of a large number of cases (1,000 cases) found that cervicogenic dizziness accounted for 89% of all dizziness, or vertigo. [5] Cervical spondylosis was one of the common causes of dizziness in the elderly in a community survey. [1] Among patients with cervical vertebral whiplash injuries, the prevalence of dizziness has been variously reported, ranging from 20% to 90%. [6] Nearly half of patients with neck pain have cervicogenic dizziness. [1] However, cervicogenic dizziness is the most controversial among all dizziness because its pathogenesis is unclear, and its diagnosis and treatment are difficult. [6-9]
Cervicogenic dizziness is considered to have four different pathogenesis, but proprioceptive cervicogenic dizziness is the most common and accepted by most scholars. [6] Unlike other forms of dizziness, cervicogenic dizziness is of interest not only to neurologists but also to physiotherapists, pain physicians, and orthopedic surgeons. The purpose of this narrative review is to highlight the pathophysiology, diagnosis, and treatment of cervicogenic dizziness from the perspective of the cervical proprioceptive afferent disorder.
There are more articles like this @



Leave A Comment