Association Between Spinal Manipulation, Butalbital Prescription, and Medication Overuse Headache in Adults With Tension-Type Headache: Retrospective Cohort Study
SOURCE: Health Science Reports 2024 (Nov 29); 7 (12): e70218
Robert J Trager • Timothy J Williamson • Pratheek S Makineni • Lindsay H Morris
Connor Whole Health University Hospitals
Cleveland Medical Center
Cleveland Ohio USA.

Background and aims: Butalbital is an acute headache medication commonly prescribed for tension-type headache (TTH), although discouraged by guidelines due to a risk of medication overuse headache (MOH). Considering spinal manipulative therapy (SMT) may reduce TTH frequency and intensity, we hypothesized adults with TTH receiving chiropractic SMT would be less likely to receive a butalbital prescription over 2 years versus matched controls not receiving SMT. We secondarily compared likelihood of MOH between cohorts.
Methods: We searched a United States medical records database of patients attending academic medical centers for adults with TTH, from 2013 to 2024, excluding those diagnosed with other headaches and seen in inpatient/emergency settings. We divided patients into two cohorts: (1) SMT and (2) non-SMT, using propensity matching to control for demographics and other variables associated with likelihood of butalbital prescription and MOH.
Results: Three thousand one hundred and sixteen patients remained per cohort after matching. The incidence of butalbital prescription was lower in the SMT cohort compared to the non-SMT cohort (SMT: 1.7%; non-SMT: 3.8%), yielding an RR (95% CI) of 0.46 (0.33-0.63; p < 0.001). The incidence of MOH was lower in the SMT cohort versus non-SMT cohort (SMT: 0.5%; non-SMT: 1.2%), yielding an RR (95% CI) of 0.44 (0.25-0.80; p < 0.001).
Conclusion: Adults receiving chiropractic SMT had a significantly lower likelihood of butalbital prescription and, tentatively, MOH compared to matched controls not receiving SMT. These findings support current guideline recommendations favoring SMT in TTH care, though future studies should replicate and compare these findings with other nonpharmacologic clinicians and interventions.
Keywords: barbiturates; chiropractic; headache; spinal manipulation.
From the FULL TEXT Article:
Background
There is more like this @
HEADACHE Section and the
NON-PHARMACOLOGIC THERAPY Section and the
INITIAL PROVIDER/FIRST CONTACT Section
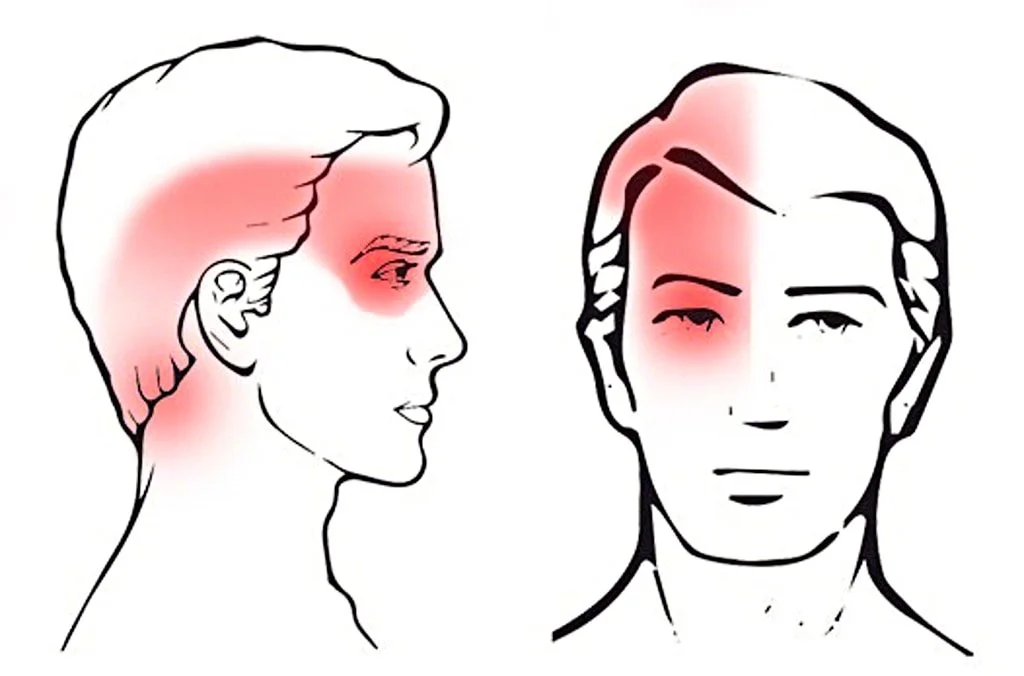
Tension-type headache (TTH) is the most common type of headache, with a global prevalence of 26%. [1, 2] TTH is typically characterized by bilateral pressing, tightening head pain, and co-occurs with neck pain in nearly 90% of patients. [3] It is occasionally treated with butalbital or butalbital-containing medications for acute/abortive purposes. [4–6] However, this has been discouraged by practice guidelines due to poor efficacy and potential complications such as withdrawal, overuse, and medication overuse headache (MOH). [2, 7–9] Patients also seek spinal manipulative therapy (SMT) for TTH relief. [10–12] While evidence supports the efficacy of SMT for TTH [13, 14], its association with butalbital prescription and MOH remains unknown. [15]
First-line medications for TTH include acetaminophen and aspirin. [3, 7, 8, 16] Butalbital, a barbiturate and sedative/hypnotic medication, is a second-line therapy but carries the risk of cognitive impairment, dependence/addiction, and headache chronification. [7, 9] In addition, patients may develop MOH, described as a worsening of the primary headache after overuse or discontinuation of acute headache medication, and occurring at least 15 days per month. [17] Common butalbital-containing medications used for headaches often include caffeine and either acetaminophen or aspirin. Butalbital-containing medications have not demonstrated efficacy for headaches in comparison to other treatments or placebo. [18]
Several studies suggest that butalbital is commonly prescribed for TTH. An examination of a US data set of ambulatory visits for nonserious, non-migraine headaches found that either opioids or barbiturates were prescribed in approximately 15% of cases. [4] According to data from a single US academic headache center, one in five patients was currently using either opioids or barbiturates, while more than half of patients had been prescribed an opioid or barbiturate [5]. Finally, another study highlighted that butalbital pr
Chiropractors are non-pharmacologic clinicians who frequently use SMT to manage musculoskeletal disorders. [11] Systematic reviews have found evidence that SMT may reduce TTH intensity and frequency compared to sham interventions or no treatment. [13, 14] In addition, SMT is recommended for TTH by the US Centers for Disease Control. [19] Considering SMT may benefit TTH, it remains plausible that patients receiving SMT may be less inclined to seek medications for acute TTH relief such as butalbital. As butalbital is not a first-line medication for TTH, examination of its prescription could reflect acute exacerbations of recalcitrant headaches and/or medication guideline non-adherence.
This study addresses gaps in the TTH literature by examining the association between SMT and butalbital prescription and MOH. We hypothesized that adults receiving chiropractic SMT for TTH would have a reduced likelihood of receiving a butalbital prescription over a 1–year follow-up compared to matched controls not receiving SMT, and secondarily compared the likelihood of MOH between cohorts.




Leave A Comment