Effect of Chiropractic Care on Low Back Pain for Active-duty Military Members: Mediation Through Biopsychosocial Factors
SOURCE: PLoS One 2024 (Oct 1); 19 (10): e0310642
Zacariah K. Shannon • Cynthia R. Long • Elizabeth A. Chrischilles • Christine M. Goertz • Robert B. Wallace • Carri Casteel • Ryan M. Carnahan
Palmer Center for Chiropractic Research,
Palmer College of Chiropractic,
Davenport, IA, USA.
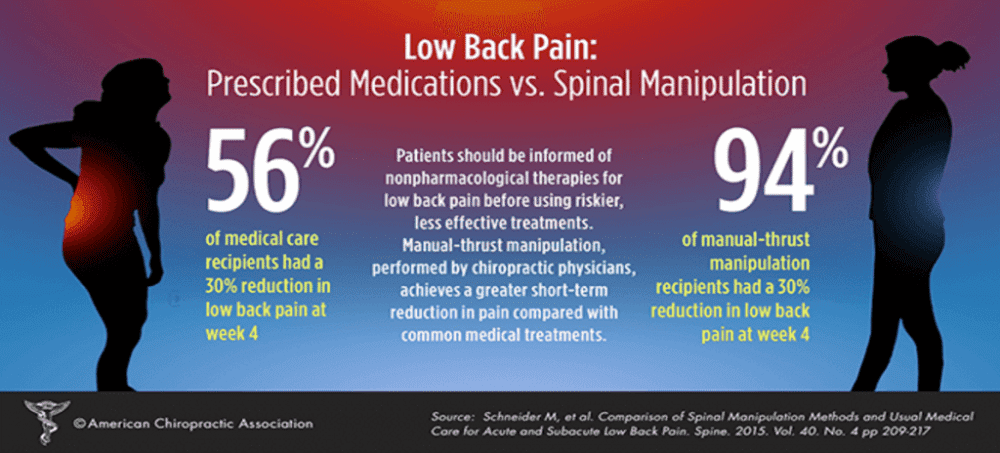
FROM: Schneider, Spine 2015
This study evaluates biopsychosocial factors as mediators of the effect of chiropractic care on low back pain (LBP) intensity and interference for active-duty military members. Data from a multi-site, pragmatic clinical trial comparing six weeks of chiropractic care plus usual medical care to usual medical care alone for 750 US active-duty military members with LBP were analyzed using natural-effect, multiple-mediator modeling. Mediation of the adjusted mean effect difference on 12-week outcomes of PROMIS-29 pain interference and intensity by 6-week mediators of other PROMIS-29 physical, mental, and social health subdomains was evaluated. The effect difference on pain interference occurring through PROMIS-29 biopsychosocial factors (natural indirect effect = -1.59, 95% CI = -2.28 to -0.88) was 56% (95% CI = 35 to 96) of the total effect (-2.82, 95% CI = -3.98 to -1.53). The difference in effect on pain intensity occurring through biopsychosocial factors was smaller (natural indirect effect = -0.32, 95% CI = -0.50 to -0.18), equaling 26% (95% CI = 15 to 42) of the total effect (-1.23, 95% CI = -1.52 to -0.88). When considered individually, all physical, mental, and social health factors appeared to mediate the effect difference on pain interference and pain intensity with mental health factors having smaller effect estimates. In contrast with effects on pain interference, much of the effect of adding chiropractic care to usual medical care for US military members on pain intensity did not appear to occur through the PROMIS-29 biopsychosocial factors. Physical and social factors appear to be important intermediate measures for patients receiving chiropractic care for low back pain in military settings. Further study is needed to determine if the effect of chiropractic care on pain intensity for active-duty military occurs through other unmeasured factors, such as patient beliefs, or if the effect occurs directly.
Trial registration registered on clinical trials.gov (NCT01692275)
From the FULL TEXT Article:
Introduction
There is more like this @ our
LOW BACK PAIN Section and the
Low back pain (LBP) is a global public health burden [1], common amongst the US general population [2], and impactful for people with physically demanding occupations. [3] Similar to other physically demanding occupations, US military members have a high risk of musculoskeletal pain, making it one of the most common reasons for interruption of combat duty. [4–6] Clinical practice guidelines recommend noninvasive and nonpharmacologic treatments as first-line therapies for LBP [7–9] which are commonly delivered as part of multi-modal chiropractic care. [10] Adding chiropractic care to usual medical care for US active-duty military members has been demonstrated to result in greater improvement in pain, disability, physical function, sleep disturbance, fatigue, anxiety, depression, and satisfaction with participation in social roles. [11, 12] The mechanisms of improvement in pain and quality-of-life when multi-modal chiropractic care is added to usual medical care are unknown, however.
Changes in pain are thought to be a result of a confluence of mechanisms. [13] To better understand a cause, it can be broken down into a set of component causes that are sufficient to produce the outcome. [14] Considering mechanisms in isolation limits the ability to understand how mechanisms fit into a component cause framework. The biopsychosocial model [15] may help elucidate pain by identifying physical, mental, and social factors as components of pain. The biopsychosocial model does not, however, provide a causal framework for evaluation. Therefore, it may be necessary to explore individual factor contributions as part of the larger framework when evaluating mechanisms. Mediation analysis is used to evaluate mechanisms of a treatment by determining how much of the effect of the treatment on the outcome occurs through intermediary variables. [16]
Understanding the mechanisms of multi-modal interventions is important to improve implementation into practice. [17] Mechanisms with large effects inform how the multi-modal intervention is currently achieving effect on outcomes, leading to opportunities to improve intervention delivery by further focusing on components targeting mechanisms with large effects and/or by better addressing potentially important mechanisms showing small effects. Evaluating the mechanisms of multi-modal interventions, such as chiropractic care, is also important if it is to be understood pragmatically, that is, when trying to understand how effects are expected to occur when patients seek care from or are referred to a chiropractor in clinical practice. Mediation analyses have been conducted to evaluate mechanisms of other multi-modal interventions such as tai-chi [18], yoga [19, 20], and physical therapy. [20, 21] The mechanisms of chiropractic care’s effect on pain have not been adequately evaluated while incorporating multiple, simultaneous component causes or in the context of the biopsychosocial model.
The objective of this study is to evaluate physical, mental, and social health factors as mechanisms of the difference in effect on LBP of usual medical care plus chiropractic care vs. usual medical care alone for active-duty military members. This study quantifies the effects of an integrative health approach to better understand how change in biopsychosocial factors contribute to change in physical pain. Our primary research question was “How much of the effect of chiropractic care on pain interference and intensity occurs through changes in other physical, mental, and social health factors?”





Leave A Comment