Spinal Pain, Chronic Health Conditions and Health Behaviors: Data from the 2016-2018 National Health Interview Survey
SOURCE: Int J Environ Res Public Health 2023 (Apr 3); 20 (7): 5369
| OPEN ACCESS |
Katie de Luca, Patricia Tavares, Haiou Yang, Eric L Hurwitz, Bart N Green, Hannah Dale, Scott Haldeman
Discipline of Chiropractic,
School of Health, Medical and Applied Science,
CQ University,
Brisbane, QLD 4701, Australia.
FROM: J Pain Res. 2021
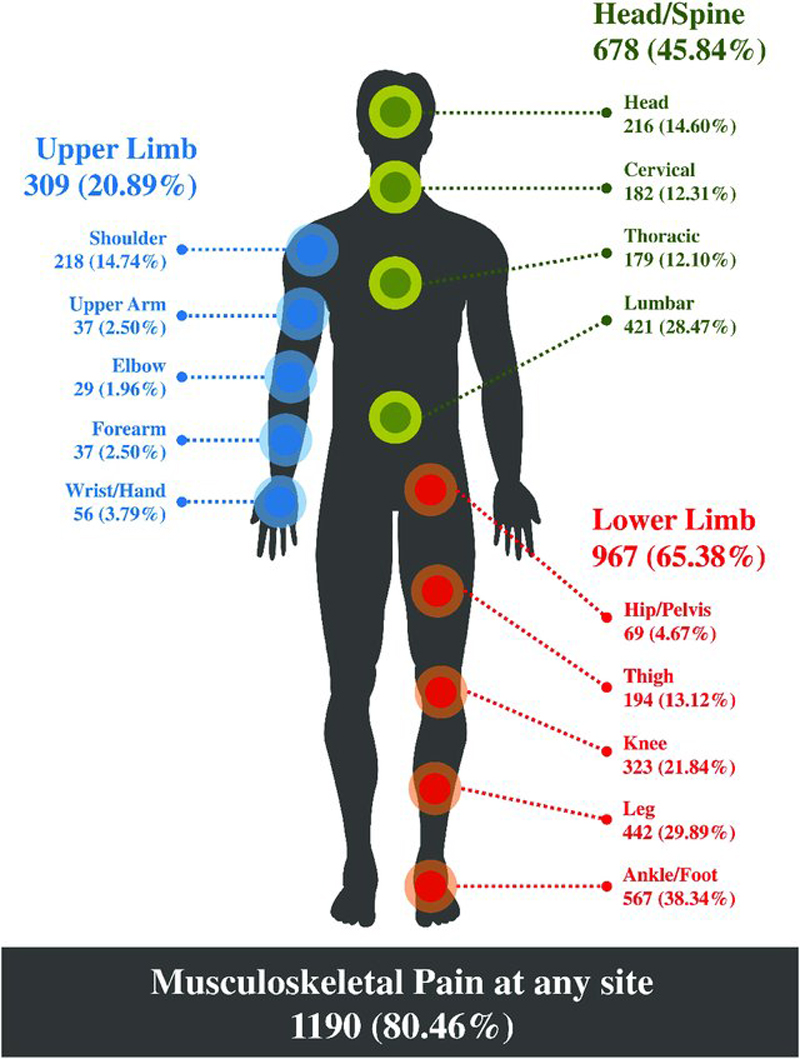
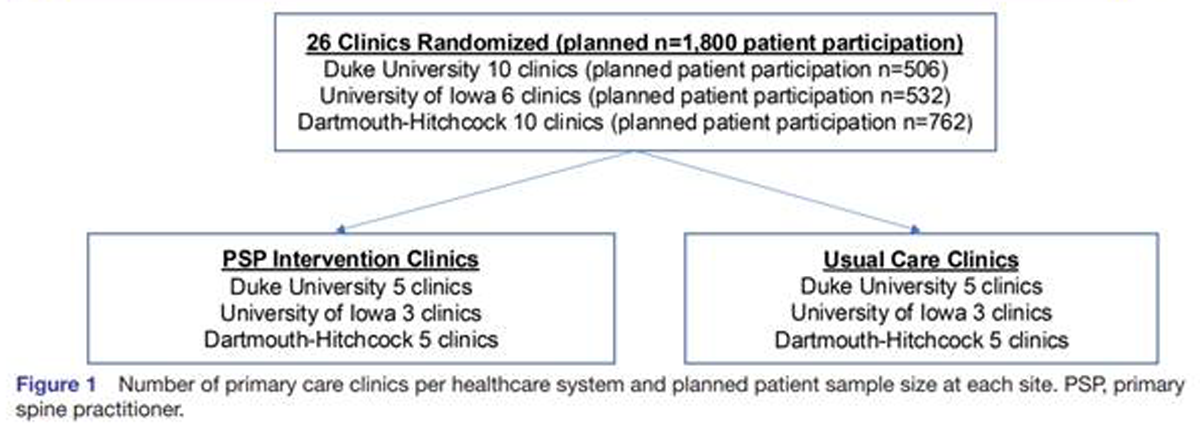
Spinal pain and chronic health conditions are highly prevalent, burdensome, and costly conditions, both in the United States and globally. Using cross-sectional data from the 2016 through 2018 National Health Interview Survey (n = 26,926), we explored associations between spinal pain and chronic health conditions and investigated the influence that a set of confounders may have on the associations between spinal pain and chronic health conditions. Variance estimation method was used to compute weighted descriptive statistics and measures of associations with multinomial logistic regression models. All four chronic health conditions significantly increased the prevalence odds of spinal pain; cardiovascular conditions by 58%, hypertension by 40%, diabetes by 25% and obesity by 34%, controlling for all the confounders.
There is more like this @ our:
LOW BACK PAIN Section and the:
CHRONIC NECK PAIN Section and the:
For all chronic health conditions, tobacco use (45–50%), being insufficiently active (17–20%), sleep problems (180–184%), cognitive impairment (90–100%), and mental health conditions (68–80%) significantly increased the prevalence odds of spinal pain compared to cases without spinal pain. These findings provide evidence to support research on the prevention and treatment of non-musculoskeletal conditions with approaches of spinal pain management.
Keywords:
back pain; cardiovascular diseases; comorbidity; diabetes mellitus; health behavior; hypertension; low back pain; neck pain; obesity; spinal pain.
From the FULL TEXT Article:
Introduction
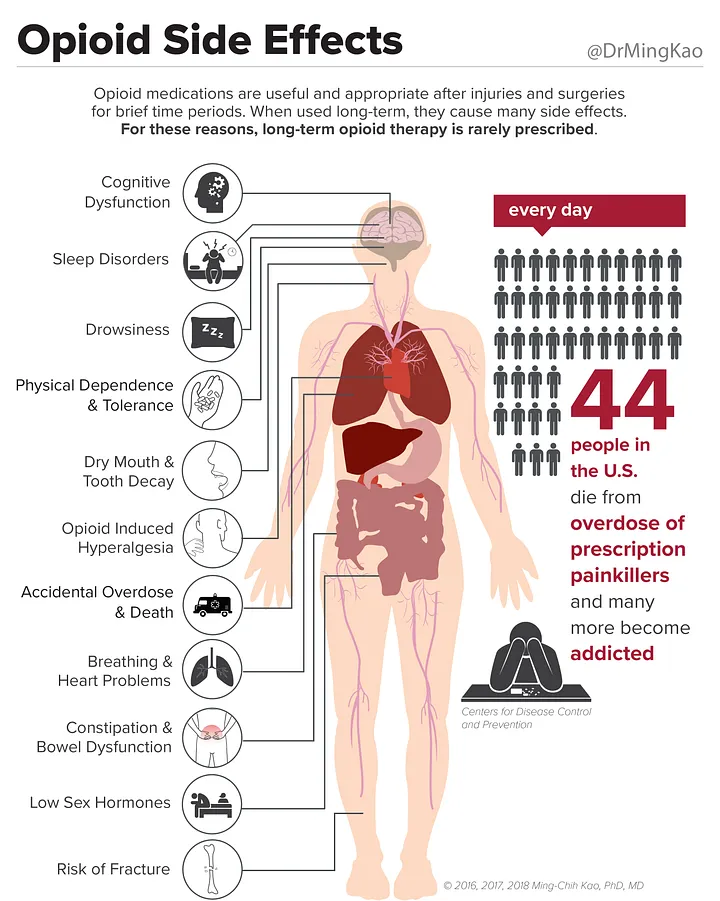
Low back and neck pain (spinal pain) are considered the leading causes of years lived with disability in most countries and age groups. [1] In the 2021 Global Burden of Disease study, low back pain continues to be the greatest cause of disability burden worldwide, with 12.5% and 11.5% of years lived with disability due to low back pain attributed to modifiable risk factors smoking and elevated body mass index, respectively. [2] In adults aged 50 years and over, low back pain, ischemic heart disease and diabetes were all ranked in the top ten causes of disability adjusted life years globally [3], with ischemic heart disease and diabetes both in the top ten causes of death globally (1st and 10th, respectively). The costs of treating these diseases are very high. Spending during the year 2020 in the US was estimated at USD 134.5 billion for low back and neck pain, USD 111.2 billion for diabetes and USD 89.3 billion for ischemic heart disease.
Several studies have reported a relationship between spinal conditions and chronic health conditions such as cardiovascular disease [4–6], hypertension [7, 8], diabetes [9, 10], and obesity. [11] A population-based study conducted in the United States reported that adult Americans with spinal pain had an increased prevalence for comorbid conditions compared with those who had low back pain only or neck pain only. [12] In Australia, a number of chronic conditions (including cardiovascular conditions, diabetes and obesity) have been shown to be associated with spinal pain in older women with arthritis, with an incremental increase in the risk of spinal pain associated with increasing comorbidity count. [13] A scoping review conducted by the Global Spine Care Initiative reported a range of health conditions such as cardiovascular disease, hypertension, diabetes and obesity associated with major categories of spinal conditions. [14]
Health behaviors have also been shown to be associated with spinal pain. In an early hallmark study on this topic, data from the 2002 US National Health Interview Survey (NHIS) revealed that current smokers, those with no leisure-time activity, and those with insomnia or trouble falling asleep were more likely to have spinal pain. [12] These findings were supported by data from the 2009–2012 NHIS, demonstrating significant associations between self-reported lower back pain and including leisure-time physical inactivity, current or former smoking, current or former alcohol drinking, and short sleep duration. [15] A biological gradient associated with exposure to smoking cigarettes and back pain was demonstrated with data from the 2012 NHIS, showing that the number of cigarettes smoked per day for current smokers was higher for those with back pain. [16]




Leave A Comment