Diagnostic Accuracy of Videofluoroscopy for Symptomatic Cervical Spine Injury Following Whiplash Trauma
SOURCE: Int J Environ Res Public Health. 2020 (Mar 5); 17 (5): E1693
Michael D. Freeman, Evan A. Katz, Scott L. Rosa, Bryan G. Gatterman, Ellen M. F. Strömmer, and Wendy M. Leith
CAPHRI School for Public Health and Primary Care,
Faculty of Health, Medicine, and Life Sciences,
Maastricht University, 6211 LM
Maastricht, The Netherlands.
BACKGROUND: Intervertebral instability is a relatively common finding among patients with chronic neck pain after whiplash trauma. Videofluoroscopy (VF) of the cervical spine is a potentially sensitive diagnostic tool for evaluating instability, as it offers the ability to examine relative intervertebral movement over time, and across the entire continuum of voluntary movement of the patient. At the present time, there are no studies of the diagnostic accuracy of VF for discriminating between injured and uninjured populations.
METHODS: Symptomatic (injured) study subjects were recruited from consecutive patients with chronic (>6 weeks) post-whiplash pain presenting to medical and chiropractic offices equipped with VF facilities. Asymptomatic (uninjured) volunteers were recruited from family and friends of patients. An ethical review and oversight were provided by the Spinal Injury Foundation, Broomfield, CO.
There are more articles like this @ our:
Radiology Page and the:
Three statistical models were utilized to assess the sensitivity, specificity, positive and negative predictive values (PPV and NPV) of positive VF findings to correctly discriminate between injured and uninjured subjects.
RESULTS: A total of 196 subjects (119 injured, 77 uninjured) were included in the study. All three statistical models demonstrated high levels of sensitivity and specificity (i.e., receiver operating characteristic (ROC) values of 0.71 to 0.95), however, the model with the greatest practical clinical utility was based on the number of abnormal VF findings. For 2+ abnormal VF findings, the ROC was 0.88 (93% sensitivity, 79% specificity) and the PPV and NPV were both 88%. The highest PPV (1.0) was observed with 4+ abnormal findings.
CONCLUSIONS: Videofluoroscopic examination of the cervical spine provides a high degree of diagnostic accuracy for the identification of vertebral instability in patients with chronic pain stemming from whiplash trauma.
KEYWORDS: digital motion x-ray; instability; positive predictive value; videofluoroscopy; whiplash
From the FULL TEXT Article:
Introduction
Neck pain is a highly prevalent condition, occurring in 10–21% of the adult population annually. [1] A frequent cause of both acute and chronic neck pain is injury from a motor vehicle crash (MVC). [2] Although a variety of spinal injuries are associated with MVCs, the most common injury type is musculoligamentous sprain or strain. [3] Such injuries often result from the type of whiplash trauma that is closely associated with rear impact crashes. The term “whiplash” refers to a traumatic whipping motion of the head and neck, primarily occurring in rear impact crashes, that produces higher peak acceleration at the head than in the neck or thoracolumbar spine. [4] While some authors have also used “whiplash” as a generic catch-all description for a variety of injuries resulting from whiplash trauma, when used to describe an injury the term generally refers to cervical spine sprain/strain injury. [5]
A well-established feature of whiplash trauma is injury to the ligaments of the cervical spine, resulting in joint laxity and instability. [6, 7] Intervertebral instability associated with ligamentous injury can be both difficult to detect and refractory to treatment. [8] Because the diagnosis of vertebral “instability” refers to an abnormality of function, the condition is typically not identifiable from static postural radiographs and may be occult to other conventional imaging (i.e., MRI and CT) and thus is prone to underdiagnosis. [9]
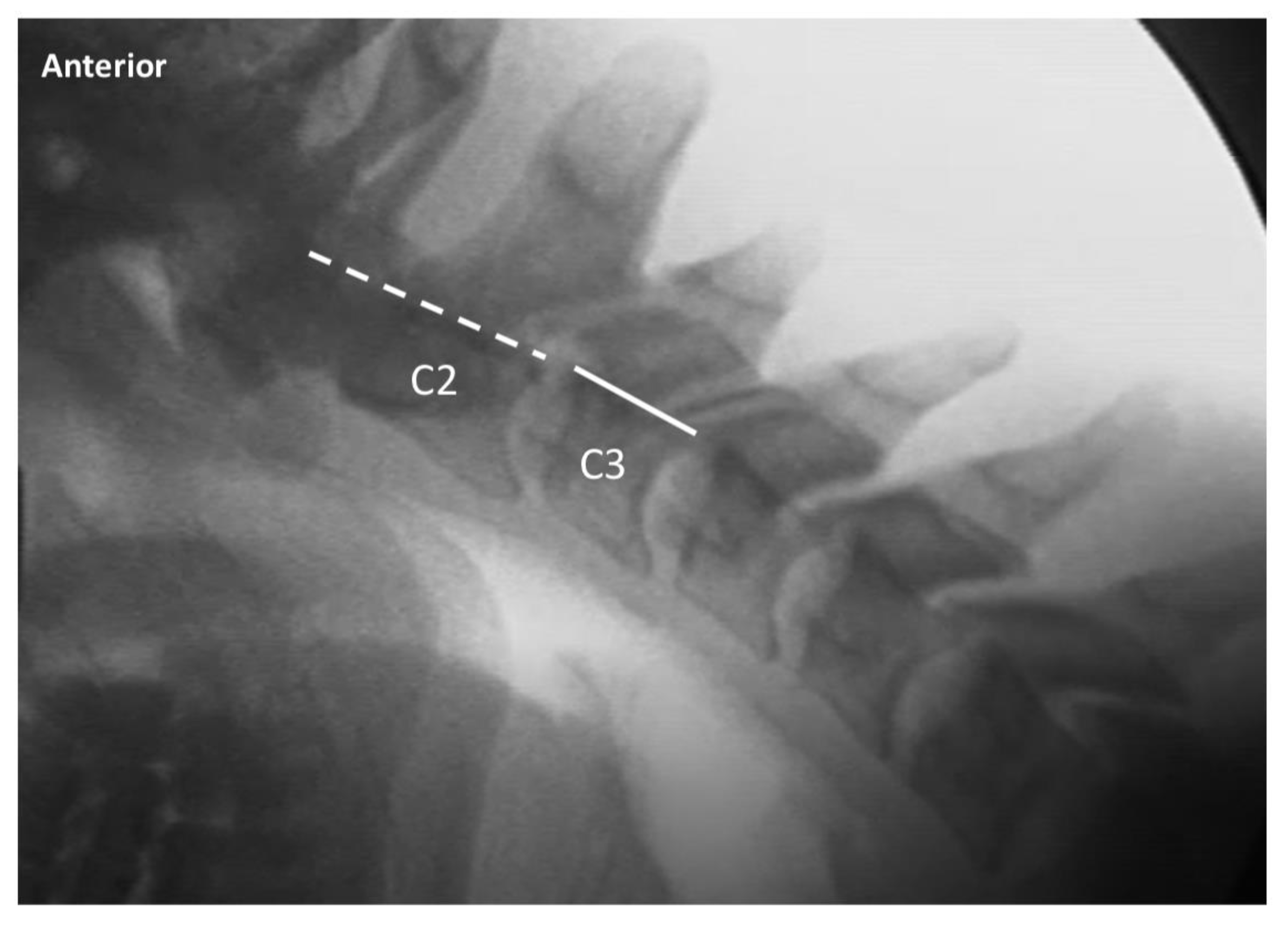
A fluoroscopic examination of the spine (also known as videofluoroscopy (VF) or digital motion x-ray (DMX)) allows for a continuous and minute examination of movement within the cervical spine, including abnormalities of intervertebral motion associated with ligamentous instability. [10] Standard VF records 30 images per second of continuous x-ray of active range of motion across multiple planes, allowing for a dynamic four-dimensional visualization of the integrity of the ligaments of the upper, mid, and lower cervical spine. [10, 11] Typically, cervical spine VF motion studies include a lateral view of flexion and extension (to examine anterior to posterior intervertebral instability) and anterior to posterior views of bilateral flexion with the mouth closed (to evaluate for excessive facet gapping in the mid and lower cervical spine) and the mouth open (to evaluate for lateral instability of C1 on C2). The studies provide evidence of the functional integrity of the ligamentum flavum, anterior and posterior longitudinal, interspinous, supraspinous and facet capsular ligaments in the mid and lower cervical spine (C2-7), and the alar and transverse ligaments in the upper cervical spine (C0-2). [7, 8, 12]
Although prior authors have examined the interrater reliability of VF for detecting cervical spine instability [13], at the present time there are no published studies describing the diagnostic accuracy (e.g., positive and negative predictive values) of VF for detecting symptomatic whiplash trauma-associated instability. The goal of the present study is therefore to provide a quantitative assessment of the ability of VF to discriminate between patients with symptomatic post-traumatic neck pain versus asymptomatic controls.
Read the rest of this Full Text article now!




Leave A Comment