Comparative Effectiveness of Usual Care With or Without Chiropractic Care in Patients with Recurrent Musculoskeletal Back and Neck Pain
SOURCE: J Gen Intern Med. 2018 (Jun 25) [Epub]
Charles Elder, MD MPH, Lynn DeBar, PhD MPH, Cheryl Ritenbaugh, PhD MPH, John Dickerson, PhD, William M. Vollmer, PhD, Richard A. Deyo, MD MPH, Eric S. Johnson, PhD, and Mitchell Haas, DC MA
Kaiser Permanente Center for Health Research,
Portland, OR, USA.
BACKGROUND: Chiropractic care is a popular alternative for back and neck pain, with efficacy comparable to usual care in randomized trials. However, the effectiveness of chiropractic care as delivered through conventional care settings remains largely unexplored.
OBJECTIVE: To evaluate the comparative effectiveness of usual care with or without chiropractic care for patients with chronic recurrent musculoskeletal back and neck pain.
STUDY DESIGN: Prospective cohort study using propensity score-matched controls.
PARTICIPANTS: Using retrospective electronic health record data, we developed a propensity score model predicting likelihood of chiropractic referral. Eligible patients with back or neck pain were then contacted upon referral for chiropractic care and enrolled in a prospective study. For each referred patient, two propensity score-matched non-referred patients were contacted and enrolled. We followed the participants prospectively for 6 months.
MAIN MEASURES: Main outcomes included pain severity, interference, and symptom bothersomeness. Secondary outcomes included expenditures for pain-related health care.
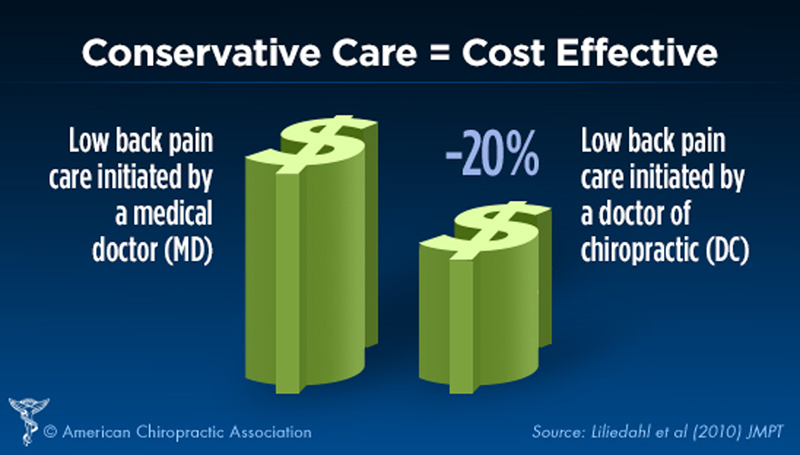
KEY RESULTS: Both groups’ (N = 70 referred, 139 non-referred) pain scores improved significantly over the first 3 months, with less change between months 3 and 6. No significant between-group difference was observed. (severity – 0.10 (95% CI – 0.30, 0.10), interference – 0.07 (– 0.31, 0.16), bothersomeness – 0.1 (– 0.39, 0.19)). After controlling for variances in baseline costs, total costs during the 6–month post-enrollment follow-up were significantly higher on average in the non-referred versus referred group ($1,996 [SD = 3874] vs $1,086 [SD = 1212], p = .034). Adjusting for differences in age, gender, and Charlson comorbidity index attenuated this finding, which was no longer statistically significant (p = .072).
There are more articles like this @ our:
CONCLUSIONS: We found no statistically significant difference between the two groups in either patient-reported or economic outcomes. As clinical outcomes were similar, and the provision of chiropractic care did not increase costs, making chiropractic services available provided an additional viable option for patients who prefer this type of care, at no additional expense.
KEYWORDS: alternative medicine; back pain; chiropractic; chronic musculoskeletal pain; comparative effectiveness; complementary and integrative medicine; managed care; neck pain; primary care; propensity scoring; spinal manipulation
From the FULL TEXT Article:
INTRODUCTION
Chronic musculoskeletal pain remains a substantial clinical and public health challenge. [1, 2] In 2008, the total financial cost of pain to society, including both health care costs and lost productivity, was estimated at $560 to $635 billion. [3] Spinal disorders are the fourth most common primary diagnosis for office visits in the USA, [4] and are reported by over a third of patients presenting with musculoskeletal complaints. [5] Conventional management commonly includes nonsteroidal antiinflammatory drugs, skeletal muscle relaxants, and opioids, which are of modest benefit and are associated with serious toxicities. [6, 7]
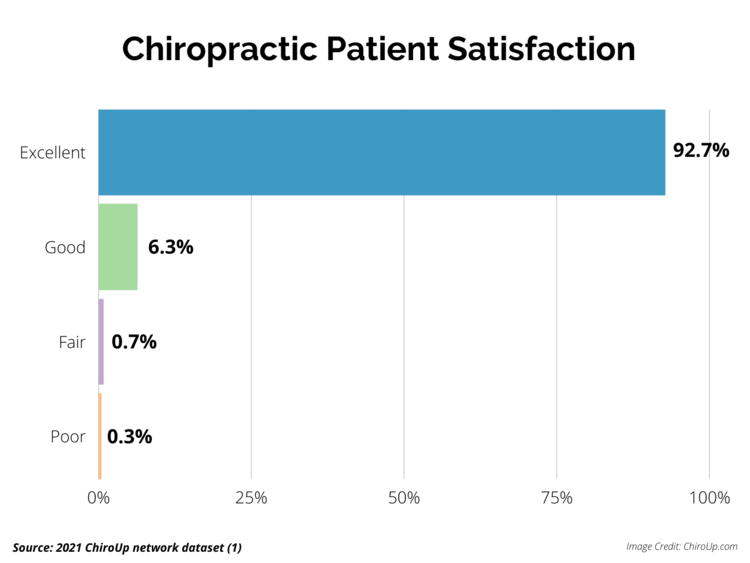
Chiropractic care is popular among patients, [8, 9] with efficacy for treating back and neck pain comparable to usual care in experimental randomized controlled trial (RCT) settings. [10–12] However, the effectiveness of chiropractic care as actually delivered in routine conventional and integrative medicine practice remains largely unexplored. Rigorous evaluation of such routine care is complicated by numerous methodological challenges. In comparative effectiveness research of this type, RCT study designs may be logistically difficult or even infeasible, where the requirements for informed consent, the mechanics of the randomization process, the protocols for blinding, and other experimental constraints often directly conflict with the flow of routine office care. Further, even if feasible, imposing these research constraints is likely to alter care as actually delivered in everyday clinical settings. Prospective cohort studies provide a compelling alternative, but introduce challenges in identifying an appropriate control group that minimizes confounding or bias.
Propensity scores represent one viable approach to controlling for confounding in observational studies. However, propensity scores are typically applied in retrospective analyses and, to our knowledge, have not been previously used to recruit and match subjects on an ongoing basis in prospective cohort studies requiring the collection of patient-reported outcomes. [13] We sought to evaluate the comparative effectiveness of usual care with or without chiropractic care as provided to patients in an established health maintenance organization (HMO), using novel and scientifically rigorous methods. Specifically, we used data from retrospective electronic health record (EHR) and administrative databases to develop a propensity score model describing the likelihood of a patient’s being referred for chiropractic care, [13] and then implemented a prospective cohort study comparing patients with chronic musculoskeletal pain who were referred for chiropractic care with propensity score-matched controls who were not.
Read the rest of this Full Text article now!



Leave A Comment