The Role of Spinal Manipulation in Addressing Disordered Sensorimotor Integration and Altered Motor Control
SOURCE: J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 768–776
Heidi Haavik, Bernadette Murphy
New Zealand College of Chiropractic,
Auckland, New Zealand.
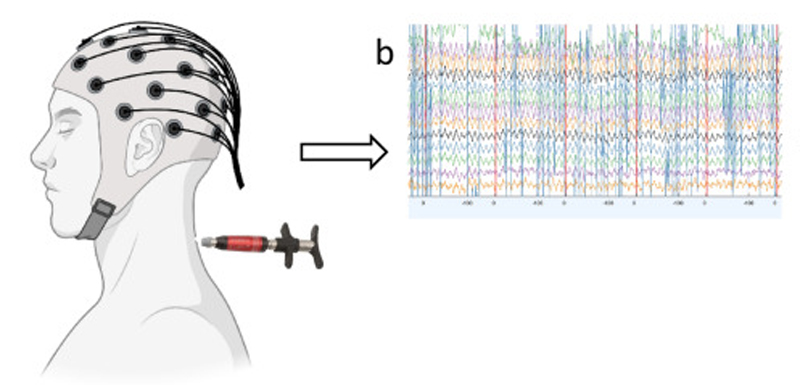
This review provides an overview of some of the growing body of research on the effects of spinal manipulation on sensory processing, motor output, functional performance and sensorimotor integration. It describes a body of work using somatosensory evoked potentials (SEPs), transcranial magnetic nerve stimulation, and electromyographic techniques to demonstrate neurophysiological changes following spinal manipulation. This work contributes to the understanding of how an initial episode(s) of back or neck pain may lead to ongoing changes in input from the spine which over time lead to altered sensorimotor integration of input from the spine and limbs.
From the Full-Text Article:
Introduction
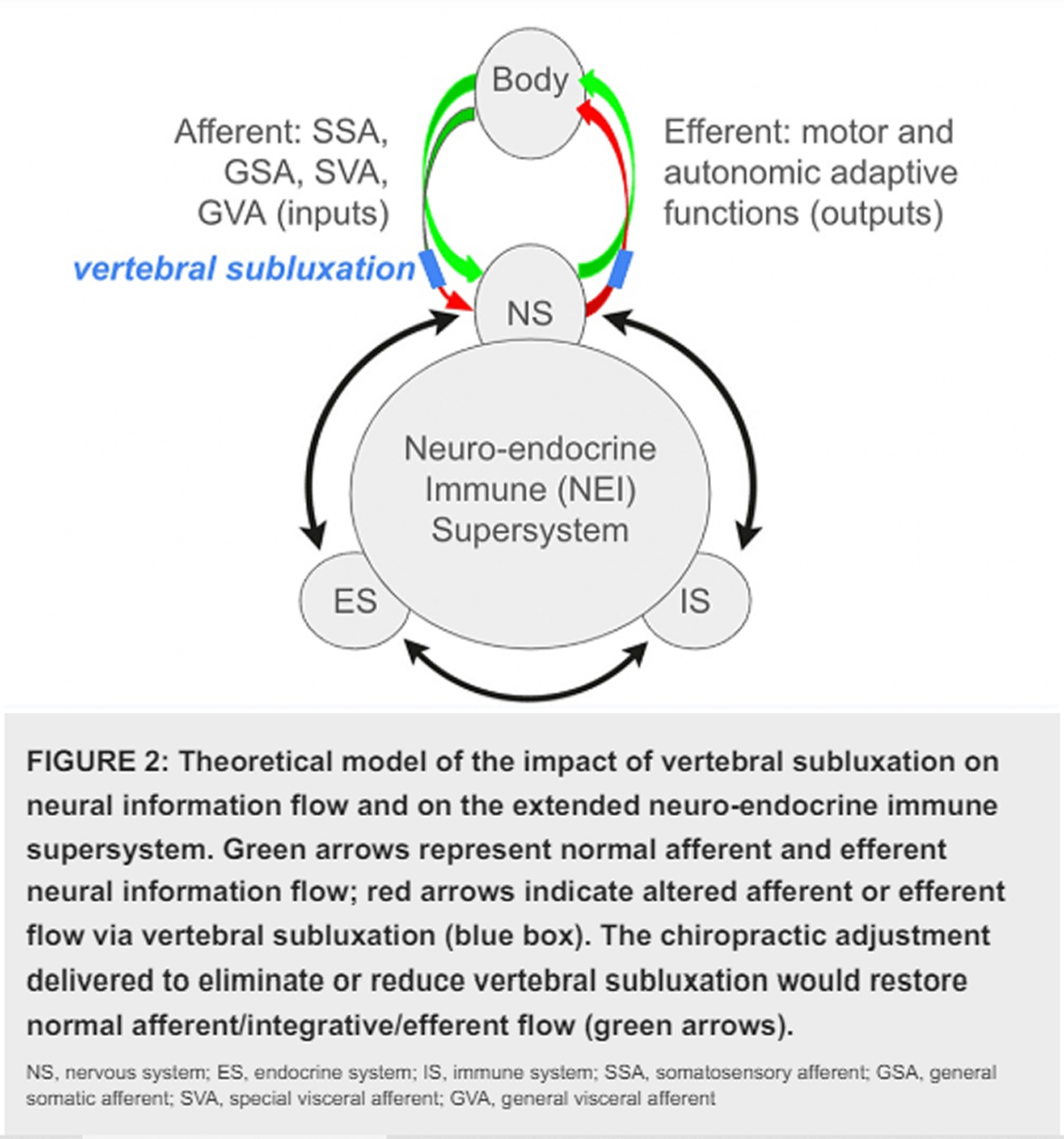
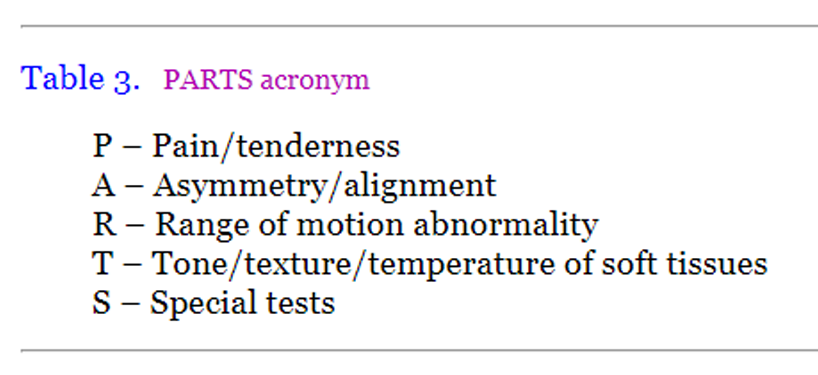
Over the past 15 years our research group has conducted a variety of human experiments that have added to our understanding of the central neural plastic effects of manual spinal manipulation (Haavik and Murphy, 2011; Haavik-Taylor and Murphy, 2007a,b, 2008, 2010c; Haavik-Taylor et al., 2010; Marshall and Murphy, 2006). Spinal manipulation is used therapeutically by a number of health professionals, all of whom have different terminology for the ‘‘entity’’ that they manipulate. This ‘‘entity’’ which generally describes areas of muscle tightness, tenderness and restricted movement may be called a ‘‘vertebral (spinal) lesion’’ by physical medicine specialists or physiotherapists, ‘‘somatic dysfunction’’ or ‘‘spinal lesion’’ by osteopaths, and ‘‘vertebral subluxation’’ or ‘‘spinal fixation’’ by chiropractors (Leach, 1986). For the purposes of this article, the ‘‘manipulable lesion’’ will be referred to as an area of spinal dysfunction or joint dysfunction. Joint dysfunction as discussed in the literature ranges from experimentally induced joint effusion (Shakespeare et al., 1985), pathological joint disease such as osteoarthritis (O’Connor et al., 1993) as well as the more subtle functional alterations that are commonly treated by manipulative therapists (Suter et al., 1999, 2000).
 |
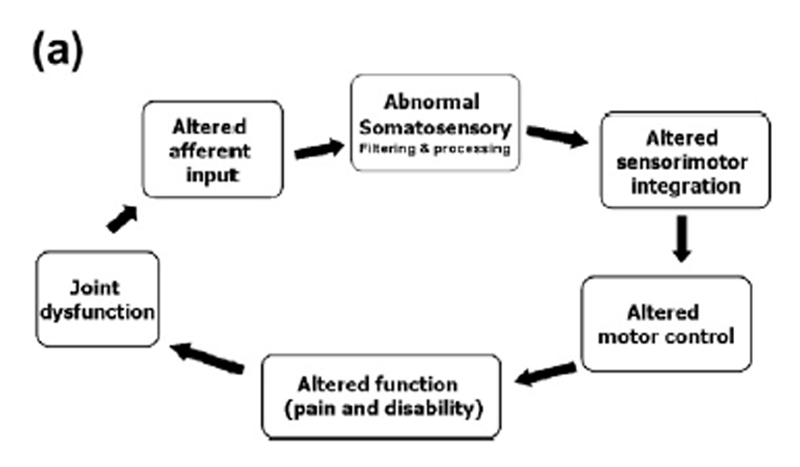
Based on our research findings we have proposed that areas of spinal dysfunction, represent a state of altered afferent input which may be responsible for ongoing central plastic changes (Haavik-Taylor et al., 2010; Haavik-Taylor and Murphy, 2007c). Furthermorewe have proposed a potential mechanism which could explain how high-velocity, low-amplitude spinal manipulation, also known as spinal adjustments, improve function and reduce symptoms. We have proposed that altered afferent feedback from an area of spinal dysfunction alters the afferent ‘‘milieu’’ into which subsequent afferent feedback from the spine and limbs is received and processed, thus leading to altered sensorimotor integration (SMI) of the afferent input, which is then normalized by highvelocity, low-amplitude manipulation (Haavik-Taylor et al., 2010; Haavik-Taylor and Murphy, 2007c). For a pictorial depiction of this hypothesis, see Figure 1.
There are more articles like this @ our:
This article will provide an overview of some of the growing body of research on the effects of spinal manipulation on sensory processing, motor output, functional performance and sensorimotor integration. This body of work contributes to our understanding of how an initial episode(s) of back or neck pain may lead to ongoing changes in input from the spine which over time lead to altered sensorimotor integration of input from the spine and limbs. Increasing this understanding may provide a neurophysiological explanation for some of the beneficial clinical effects reported by chiropractors and other manipulative therapists in day to day practice. Chronic musculoskeletal pain affects the lives of millions of individuals and places a great burden on health care systems in the western world. Some of the research discussed in this review has the potential to identify objective neurophysiological markers which may be able to predict which patients will respond best to spinal manipulative treatment and/or whether a patient has had a sufficient amount of treatment to normalize neurophysiological markers of disordered sensorimotor integration. The relationship between the development and maintenance of chronic musculoskeletal pain and neural markers of altered function is a promising area in need of further research.
Read the rest of this Full Text article now!

Leave A Comment