The Comparative Prognostic Value of Directional Preference and Centralization: A Useful Yool for Front-line Clinicians?
SOURCE: J Man Manip Ther. 2008; 16 (4): 248–254
Audrey Long, BSc, PT, Stephen May, MSc, and Tak Fung, PhD
Senior Statistical Consultant,
University of Calgary,
Calgary AB, Canada.
A large number of prognostic factors have been associated with recovery from an episode of back pain, and much emphasis has been placed on psychosocial prognostic factors. The large number of prognostic factors and the lack of comparative analysis of different factors make use of these difficult in clinical practice. The aim of this study was to evaluate the comparative usefulness of a range of factors to predict outcome using data from a randomized controlled trial (RCT) in which 312 patients with sub-acute to chronic back pain received a mechanical evaluation and were sub-grouped based on the presence or absence of directional preference (DP). Patients were then randomized to treatment that was matched or unmatched to that DP.
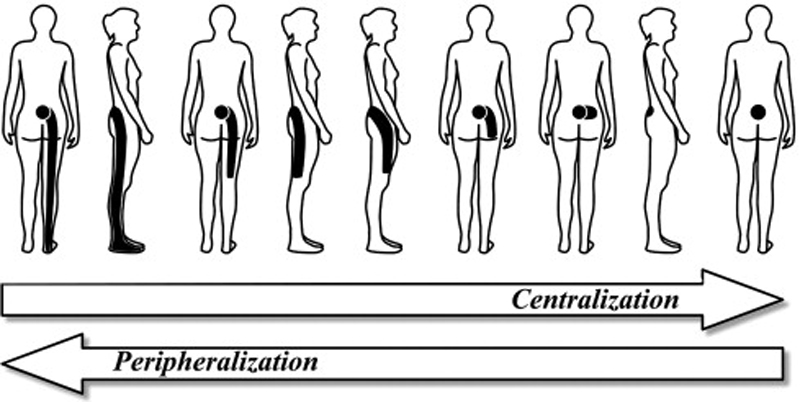
Patients with a minimal reduction of 30% in Roland-Morris Disability Questionnaire (RMDQ) score were defined as the good outcome group. Seventeen baseline variables were entered into a step-wise logistic regression analysis for the ability to predict a good outcome. Of the patients, 84 met the good outcome criteria and had a mean RMDQ decrease of 58.2% (9.8 points) in 4 visits. Leg pain, work status, depression, pain location, chronicity, and treatment assignment were significant predictors of outcome in univariate analysis. Only leg bothersomeness rating and treatment assignment survived multivariate analysis. Subjects with DP/centralization who received matched treatment had a 7.8 times greater likelihood of a good outcome. Matching patients to their DP is a stronger predictor of outcome than a range of other biopsychosocial factors.
There are more articles like this @ our:
KEYWORDS: Centralization; McKenzie Method; Mechanical Low Back Pain; Multivariate Regression Analysis; Prognosis
From the FULL TEXT Article:
Introduction
Low back pain (LBP) is extremely common both in the general population and in those seeking healthcare. [1–8] Point prevalence estimates for LBP are at least 20% of the general population [2, 5, 6]; yearly prevalence estimates are at least 40% [1–4, 8]; and lifetime prevalence is around 60%. [2, 3, 6, 8] In contrast to earlier claims [9] of a relatively benign natural history for acute back pain, it is now clear that LBP is commonly both highly recurrent and frequently persistent [10, 11]. These systematic reviews on the topic noted that after initial improvements, there is little further improvement after 3 months, at which point approximately 50% are still experiencing activity limitation; in addition, 66–75% of patients have at least one recurrence within 12 months [10, 11]. Not surprisingly, the direct and indirect costs associated with such a common, activity limiting, persistent, and episodic problem are vast in many developed countries. [12–14] Treatments seem to have been largely ineffective at altering this “20th-century medical disaster”. [15]
Given the now documented high prevalence rate, and the persistent and recurrent nature of LBP, there has been considerable recent interest in determining prognostic factors that might affect the outcome of an episode of LBP. Understanding prognostic factors would help to shape relevant management strategies and assist with early identification of individuals at high risk of developing chronic pain and disability. Ultimately, the goal would be to refine treatment approaches and permit the wiser allocation of scarce health care resources and the prevention of chronic problems. [16] Equally, identification of patients likely to have an uncomplicated recovery would help prevent overuse of healthcare resources by those who least need it. [16]
Read the rest of this Full Text article now!


Leave A Comment