Conservative Spine Care: Opportunities to Improve the Quality and Value of Care
SOURCE: Popul Health Manag. 2013 (Dec); 16 (6): 390–396
Thomas M. Kosloff, DC, David Elton, DC, Stephanie A. Shulman, DVM, MPH, Janice L. Clarke, RN, Alexis Skoufalos, EdD, and Amanda Solis, MS
Physical Health, Optum Health,
Kingston, New York.
Low back pain (LBP) has received considerable attention from researchers and health care systems because of its substantial personal, social, work-related, and economic consequences. A narrative review was conducted summarizing data about the epidemiology, care seeking, and utilization patterns for LBP in the adult US population. Recommendations from a consensus of clinical practice guidelines were compared to findings about the current state of clinical practice for LBP. The impact of the first provider consulted on the quality and value of care was analyzed longitudinally across the continuum of episodes of care. The review concludes with a description of recently published evidence that has demonstrated that favorable health and economic outcomes can be achieved by incorporating evidence-informed decision criteria and guidance about entry into conservative low back care pathways.
From the FULL TEXT Article:
Introduction
The united states has the most expensive and complex health care system in the world, [1] yet the magnitude of funds spent on the system has failed to provide commensurate benefits in terms of quality, access, and cost performance. [2]
There are more articles like this @ our:
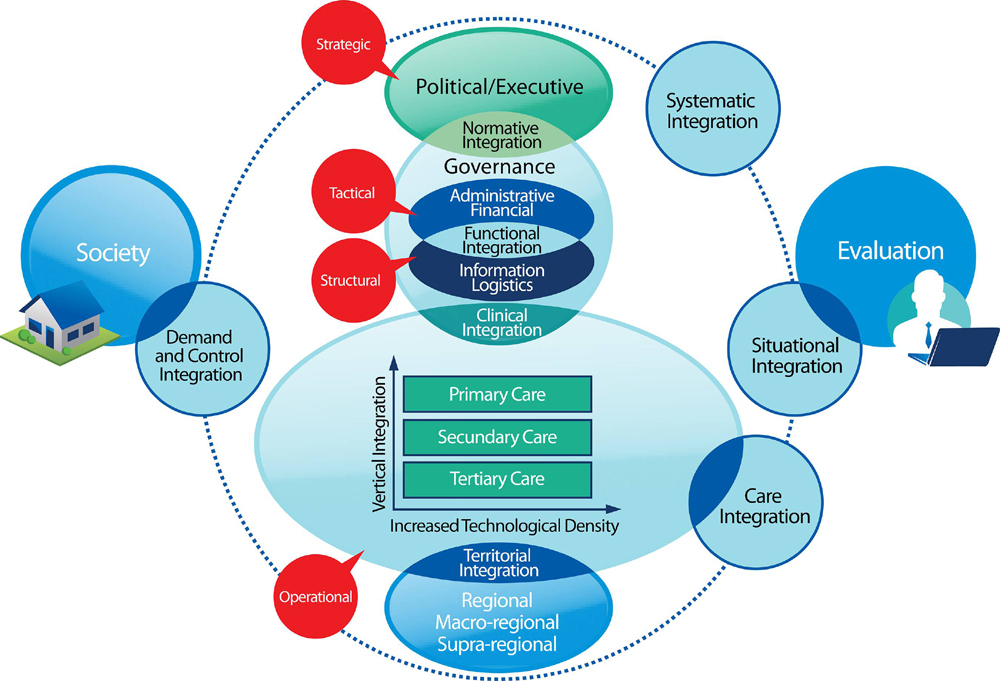
To achieve value for the current levels of investment in care, the factors that contribute to variation in costs and quality must be addressed. In fact, experts have concluded that the quality and efficiency of the US health care system could be improved by approaches that address overuse, and inappropriate or ineffective use of care — the chief factors contributing to the current high levels of expenditures, inefficiency, and waste. [3]
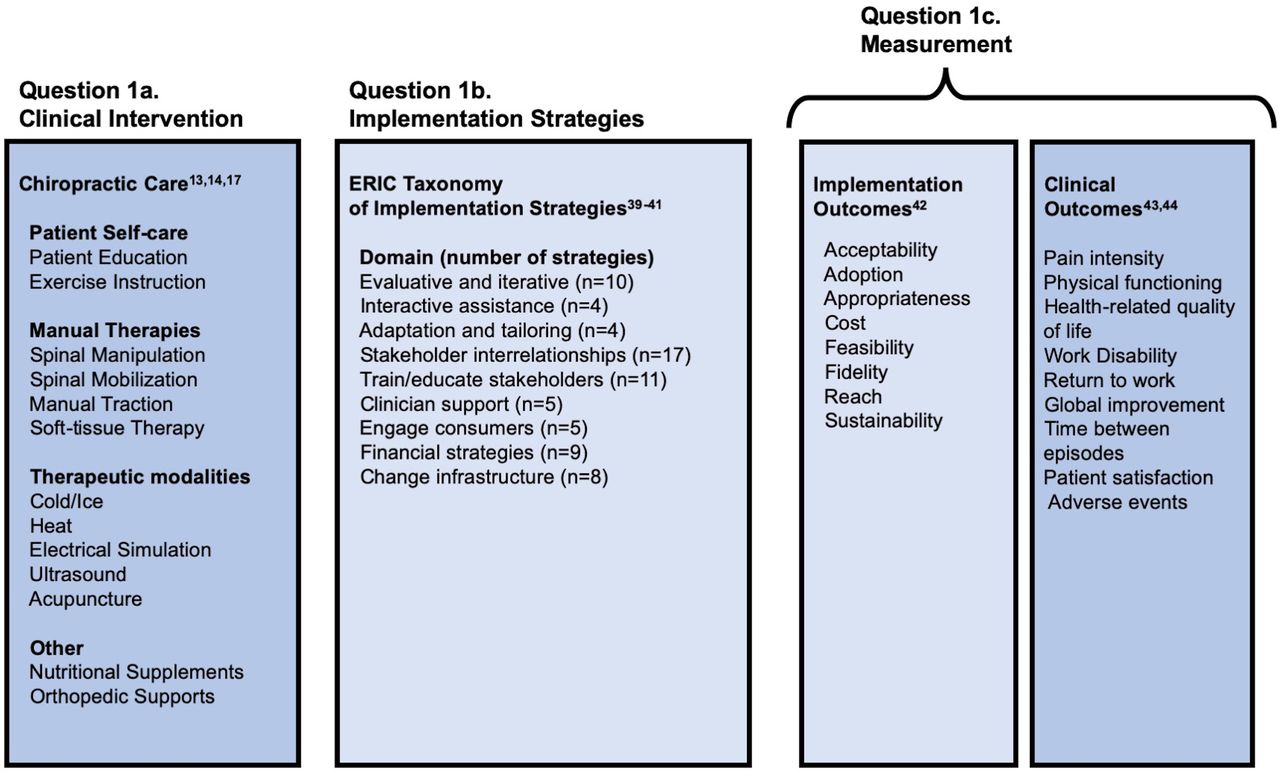
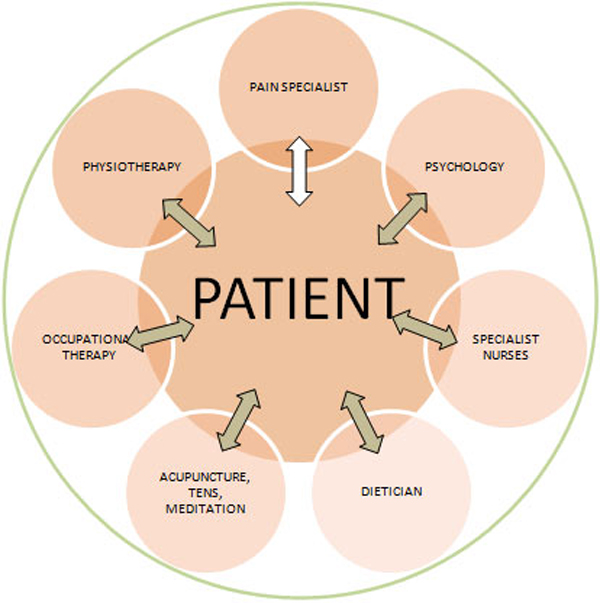
A previous article analyzed current practices regarding the use of coronary stents in the chronic stable angina patient. [4] Musculoskeletal disorders represent another diagnostic class that, while usually not life threatening, results in a high prevalence of morbidity and significant societal burden. [5] Low back pain (LBP) management in particular has been linked to inefficiency and waste. [6] This is likely related, in part, to the growing list of treatment approaches recommended for conservative care (pharmacologic and non-pharmaceutical options) and the difficulty in determining the best option for each patient. [7]
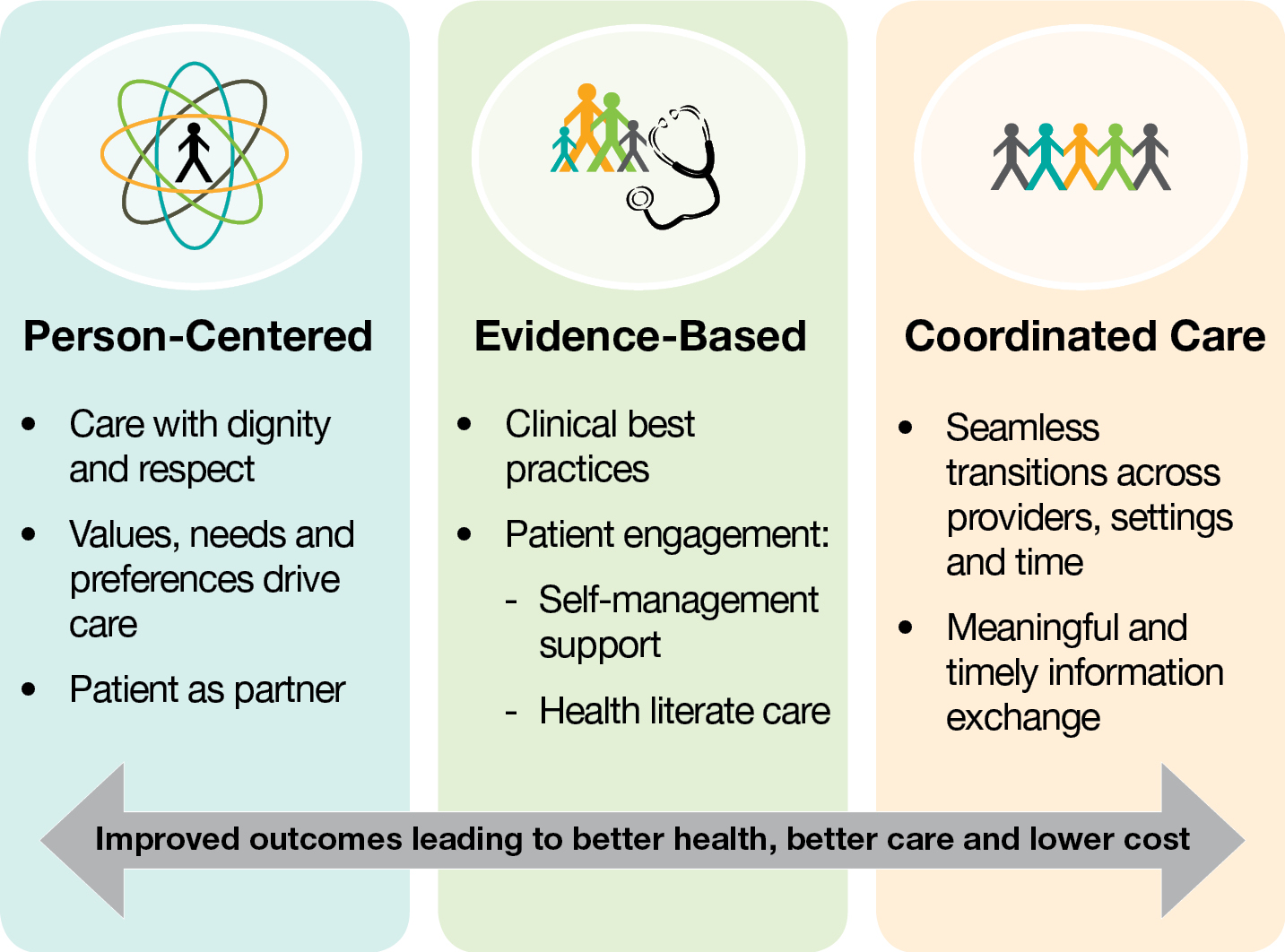
Although useful in assisting practitioner and patient decisions about appropriate health care for specific clinical circumstances, [8] clinical practice guidelines (CPGs) are not sufficient to maximize effectiveness and cost-effectiveness at the individual level (ie, targeting specific care). [9] The clinical appropriateness of health care services at the individual level can be assessed by considering the patient’s clinical characteristics, the relevant risk factors, the setting or health care provider type, the severity of the illness, and the specific requirements for a procedure (eg, availability of the service). [9]
The purpose of this article is to discuss the challenges associated with management of LBP and describe an evidence-informed process to effectively and cost-effectively integrate individual patient conservative care for LBP with appropriate population-based recommendations found in high-quality CPGs.
Read the rest of this Full Text article now!


Leave A Comment