A Modern Neuroscience Approach to Chronic Spinal Pain:
Combining Pain Neuroscience Education with Cognition-targeted Motor Control Training
SOURCE: Phys Ther. 2014 (May); 94 (5): 730–738
Jo Nijs, Mira Meeus, Barbara Cagnie, Nathalie A. Roussel, Mieke Dolphens, Jessica Van Oosterwijck, Lieven Danneels
Pain in Motion Research Group,
Departments of Human Physiology and Physiotherapy,
Faculty of Physical Education & Physiotherapy,
Vrije Universiteit
Brussels, Belgium
Chronic spinal pain (CSP) is a severely disabling disorder, including nontraumatic chronic low back and neck pain, failed back surgery, and chronic whiplash-associated disorders. Much of the current therapy is focused on input mechanisms (treating peripheral elements such as muscles and joints) and output mechanisms (addressing motor control), while there is less attention to processing (central) mechanisms. In addition to the compelling evidence for impaired motor control of spinal muscles in patients with CSP, there is increasing evidence that central mechanisms (ie, hyperexcitability of the central nervous system and brain abnormalities) play a role in CSP. Hence, treatments for CSP should address not only peripheral dysfunctions but also the brain. Therefore, a modern neuroscience approach, comprising therapeutic pain neuroscience education followed by cognition-targeted motor control training, is proposed. This perspective article explains why and how such an approach to CSP can be applied in physical therapist practice.
From the FULL TEXT Article:
Introduction
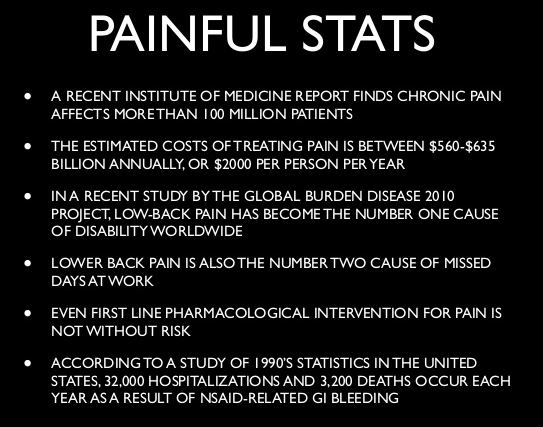
Chronic spinal pain (CSP) includes nonrecurrent chronic low back pain, failed back surgery, chronic whiplash-associated disorders, and chronic nontraumatic neck pain, among other conditions, and accounts for a large proportion of the chronic pain population. [1] Chronic spinal pain is a severely disabling disorder characterized by tremendous personal and socioeconomic impact, with long-term sick leave, low quality of life, and very high socioeconomic costs. [2]
There are more articles like this @ our:
Within the context of the management of painful musculoskeletal disorders, it is crucial to consider the concept of pain mechanisms. [3]
Pain mechanisms have been broadly categorized into:
(1) input mechanisms, including nociceptive pain and peripheral neurogenic pain;
(2) processing mechanisms, including central pain and central sensitization and the cognitive-affective mechanisms of pain; and
(3) output mechanisms, including autonomic, motor, neuroendocrine, and immune systems. [4]
Except for inflammatory pain conditions (eg, rheumatoid arthritis) or noninflammatory sources of ongoing spinal nociception, the stage of real tissue damage or nociception has disappeared in CSP. Within this context, there is increasing evidence that central mechanisms (ie, brain abnormalities [changes in brain structure and function] and hyperexcitability of the central nervous system [sensitization of the brain]) play a tremendous role in patients with CSP.
Brain atrophy, especially decrease in the density of brain gray matter (containing the neural cell bodies), [5–10] has been shown repeatedly in patients with chronic low back pain. Besides brain atrophy, descending pain inhibition or brain-orchestrated analgesia is malfunctioning in people with CSP. [11–14] The latter suggests a cardinal role for hyperexcitability of the central nervous system, or central sensitization, in patients with CSP. Many patients with CSP show features of central sensitization, [2, 11, 13–22] which is operationally defined as “an amplification of neural signalling within the central nervous system that elicits pain hypersensitivity.” [23](pS2)
Read the rest of this Full Text article now!




Leave A Comment