Will Shared Decision Making Between Patients with Chronic Musculoskeletal Pain and Physiotherapists, Osteopaths and Chiropractors Improve Patient Care?
SOURCE: Fam Pract. 2012 (Apr); 29 (2): 203–212
S Parsons, G Harding, A Breen, N Foster,
T Pincus, S Vogel and M Underwood
Department of Infectious Disease Epidemiology,
School of Public Health,
Imperial College School of Medicine,
Imperial College London,
London, UK.
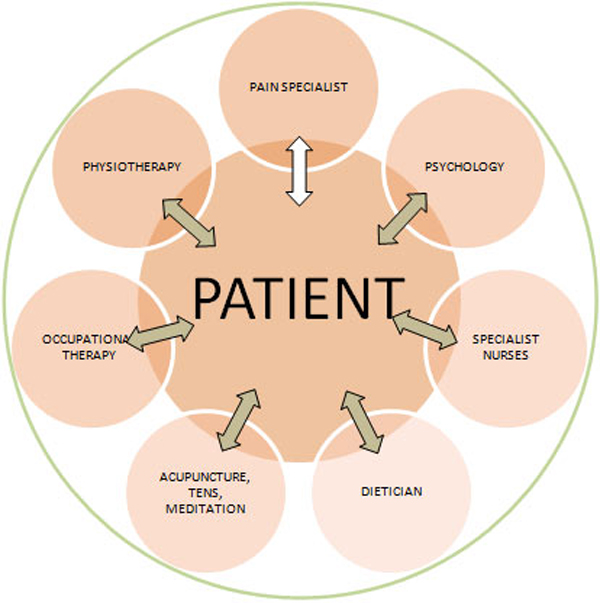
BACKGROUND: Chronic musculoskeletal pain (CMP) is treated in primary care by a wide range of health professionals including chiropractors, osteopaths and physiotherapists.
AIMS: To explore patients and chiropractors, osteopaths and physiotherapists’ beliefs about CMP and its treatment and how these beliefs influenced care seeking and ultimately the process of care.
METHODS: Depth interviews with a purposive sample of 13 CMP patients and 19 primary care health professionals (5 osteopaths, 4 chiropractors and 10 physiotherapists).
RESULTS: Patients’ models of their chronic musculoskeletal pain (CMP) evolved throughout the course of their condition. Health professionals’ models also evolved throughout the course of their treatment of patients. A key influence on patients’ consulting behaviour appeared to be finding someone who would legitimate their suffering and their condition. Health professionals also recognized patients’ need for legitimation but often found that attempts to explore psychological factors, which may be influencing their pain could be construed by patients as delegitimizing. Patients developed and tailored their consultation strategies throughout their illness career but not always in a strategic fashion. Health professionals also reflected on how patients’ developing knowledge and changing beliefs altered their expectations. Therefore, overall within our analysis, we identified three themes: ‘the evolving nature of patients and health professionals models of understanding CMP’; ‘legitimating suffering’ and ‘development and tailoring of consultation and treatment strategies throughout patients’ illness careers’.
There are more articles like this @ our:
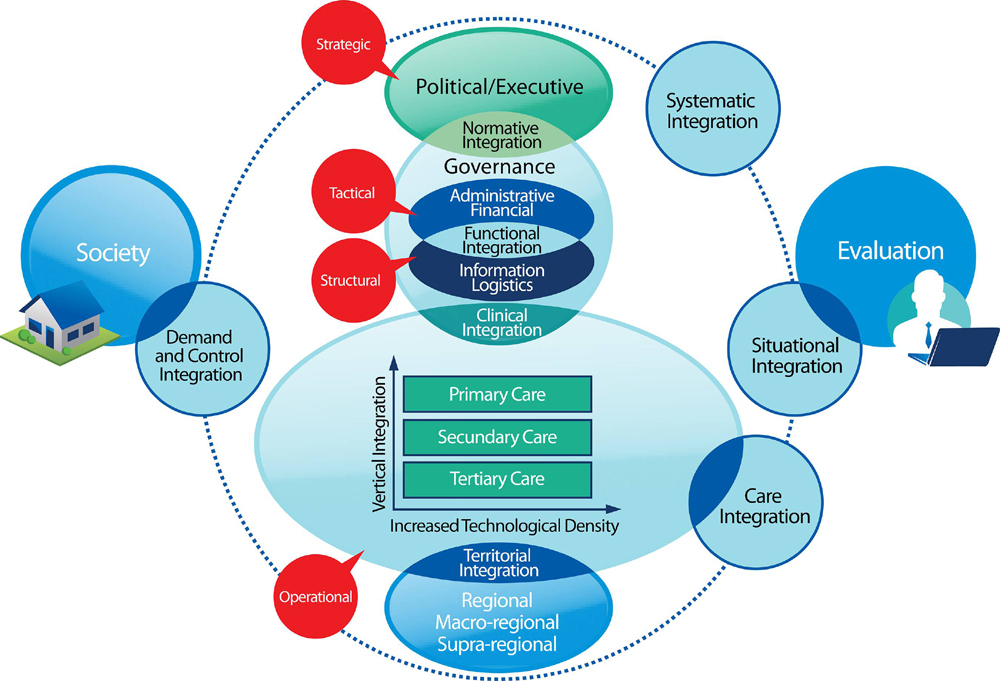
Integrated Health Care Page and the:
CONCLUSIONS: Seeking care for any condition is not static but a process particularly for long-term conditions such as chronic musculoskeletal pain (CMP). This may need to be taken into account by both CMP patients and their treating health professionals, in that both should not assume that their views about causation and treatment are static and that instead they should be revisited on a regular basis. Adopting a shared decision-making approach to treatment may be useful particularly for long-term conditions; however, in some cases, this may be easier said than done due to both patients’ and health professionals’ sometimes discomfort with adopting such an approach. Training and support for both health professionals and patients may be helpful in facilitating a shared decision-making approach.
Keywords: Beliefs, health professionals, pain, patients, qualitative
From the FULL TEXT Article:
Background
Chronic musculoskeletal pain (CMP) is a complex and costly health problem, which is treated by a wide range of health professionals [National Health Service (NHS) and private, mainstream and complementary]. [1] Despite the range of treatment options available, it appears to be difficult to treat CMP to the satisfaction of both patients and health professionals. [2] As part of a programme of research exploring the process of care for CMP, we undertook a systematic review in which we reviewed studies exploring the influence of patients’ and health professionals’ beliefs and expectations about CMP and its treatment on the process of the primary care consultation. [3] Within this programme of work, we defined the process of care as looking at the patients’ perception of their problem, its management and the dynamic interaction between the condition, the patients’ perception and the practitioners’ influence. [4]
Within the review, we found that the eligible studies primarily focused on GPs and that the lack of satisfaction reported by patients and health professionals may be due to both incorrectly ‘second-guessing’ one another’s expectations, presenting mismatching understandings of the patients’ pain to one another and perceiving that each is making unrealistic demands. [3] Therefore, we found that the majority of previous work had mainly explored the GP perspective despite a wide range of physical therapists also being consulted by patients with chronic pain, and so, we felt that it would also be important to explore the perspectives of these practitioners.
Within this study, we aimed to explore patients and chiropractors, osteopaths and physiotherapists’ beliefs about CMP and its treatment and how these beliefs influenced care seeking and ultimately the process of care.
Within this paper, we have focused on exploring themes about the overall process of care rather than on patients’ experiences of receiving care from a particular professional group.
SOURCE: Read the rest of this Full Text article now!


Leave A Comment