Perspectives of Older Adults on Co-management of Low Back Pain by Doctors of Chiropractic and Family Medicine Physicians: A Focus Group Study
SOURCE: BMC Complement Altern Med. 2013 (Sep 16); 13: 225
Kevin J Lyons, Stacie A Salsbury, Maria A Hondras, Mark E Jones, Andrew A Andresen and Christine M Goertz
Palmer Center for Chiropractic Research,
Palmer College of Chiropractic,
Davenport, IA, USA.
BACKGROUND: While older adults may seek care for low back pain (LBP) from both medical doctors (MDs) and doctors of chiropractic (DCs), co-management between these providers is uncommon. The purposes of this study were to describe the preferences of older adults for LBP co-management by MDs and DCs and to identify their concerns for receiving care under such a treatment model.
METHODS: We conducted 10 focus groups with 48 older adults who received LBP care in the past year. Interviews explored participants’ care seeking experiences, co-management preferences, and perceived challenges to successful implementation of a MD–DC co-management model. We analyzed the qualitative data using thematic content analysis.
RESULTS: Older adults considered LBP co-management by MDs and DCs a positive approach as the professions have complementary strengths. Participants wanted providers who worked in a co-management model to talk openly and honestly about LBP, offer clear and consistent recommendations about treatment, and provide individualized care. Facilitators of MD–DC co-management included collegial relationships between providers, arrangements between doctors to support interdisciplinary referral, computer systems that allowed exchange of health information between clinics, and practice settings where providers worked in one location. Perceived barriers to the co-management of LBP included the financial costs associated with receiving care from multiple providers concurrently, duplication of tests or imaging, scheduling and transportation problems, and potential side effects of medication and chiropractic care. A few participants expressed concern that some providers would not support a patient-preferred co-managed care model.
There are more articles like this @ our:
Senior Care Page and the:
Low Back Pain Page and the:
CONCLUSIONS: Older adults are interested in receiving LBP treatment co-managed by MDs and DCs. Older adults considered patient-centered communication, collegial interdisciplinary interactions between these providers, and administrative supports such as scheduling systems and health record sharing as key components for successful LBP co-management.
Keywords: Older adults, Low back pain, Health services for the aged, Interprofessional relations, Chiropractic, Family medicine, Musculoskeletal disorders, Complementary/alternative medicine, Patient preferences, Qualitative research
From the FULL TEXT Article:
Background
Low back pain (LBP) is a leading cause of disability and disease burden. [1, 2] People age 65 years and older report a 25% monthly LBP prevalence rate [3, 4] with recurrent or debilitating LBP common in older populations. [4-6] Chronic LBP is linked to difficulties with activities of daily living (ADLs) [7, 8], depression [4, 7, 9, 10], sleep problems [7, 9], and decreased performance on physical function [7, 11] and neuropsychological tests. [11] An estimated 2.3% of annual physician visits in the U.S. are for LBP. [3] Persons with LBP and other spine conditions have increased healthcare expenditures for medications, spinal imaging, injections and surgery [3, 4, 9, 12-14]. Medicare charges among older adults with back disorders have demonstrated significant increases for patient visits, imaging and spinal injections [12, 15] without translation to better health outcomes for LBP patients. [13-15]
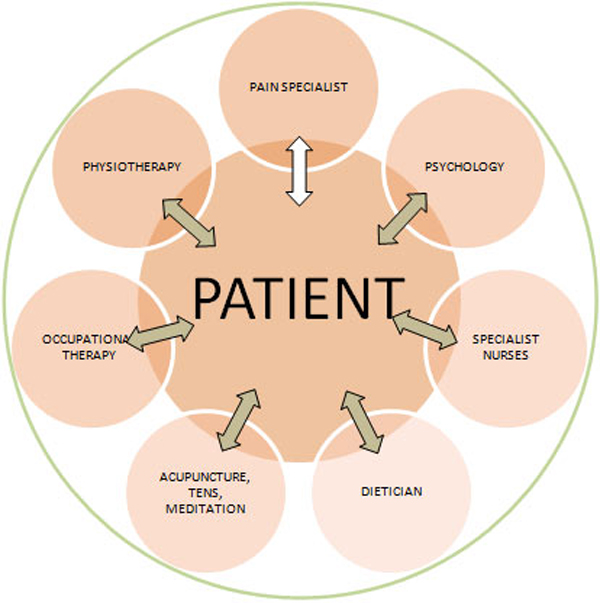
Patients with unresolved pain may pair conventional healthcare with complementary and alternative medicine (CAM). [16-19] Chiropractic is among the most widely used CAM therapies [16, 17, 20, 21], including by older adults. [22-26] Patients who use medical care and chiropractic together believe the combination helps their condition more than either alone. [21] And yet, co-occurring medical and chiropractic care is uncommon among older patients, ranging from 5-11% [23] to 33%. [27] Medical doctors (MDs) and doctors of chiropractic (DCs) make few formal referrals to each other and rarely share health records, suggesting little care coordination between these providers. [28-30] While patients of all ages might benefit from improved co-management of their pain and other medical conditions [31-33], interprofessional collaboration between healthcare providers is particularly important for older adults due to the high rates of chronic disease, multimorbidity and disability [32, 34-36], polypharmacy [37, 38], and healthcare received from multiple providers [39] in this patient population.
The purpose of this focus group study was to explore the perspectives of older adults toward LBP collaborative care by MDs and DCs. Researchers have conducted focus groups to understand patients’ LBP experiences [40, 41] and primary care preferences [42, 43] and to design interventions for musculoskeletal disease. [44-47] However, researchers have not explored the patient perspective on LBP collaborative care. In this paper, we describe older adults’ LBP healthcare seeking experiences, expectations for collaborative care provided by family medicine MDs and DCs, and insights into implementation barriers and facilitators. We incorporated the recommendations from these focus groups into the design of an interdisciplinary model and training plan for DCs and MDs providing co-managed LBP care to older people that was subsequently tested in a pragmatic randomized controlled trial. [48]
Read the rest of this Full Text article now!


Leave A Comment