My Rotation Through a VA Pain Medicine Clinic
SOURCE: ACA News ~ January 29, 2018
By Stephanie Halloran, DC
Part of a series on the chiropractic residency program in the VA health care system
Some of the most valuable knowledge you gain in the Veterans Affairs (VA) chiropractic residency program comes from rotating in other specialties. Within the VA Connecticut Healthcare System, I rotate at both the West Haven and Newington locations. Thus far, I have spent time in rheumatology, physiatry, women’s clinic (primary care), neurology, pain medicine and the interventional pain clinic. Although each rotation has contributed greatly to my clinical acumen, this post will primarily focus on pain medicine.
 |
Pain medicine is a medical subspecialty generally comprised of anesthesiologists, physiatrists or neurologists who have completed an additional one-year post-residency fellowship. As the name implies, these specialists manage overall pain with a goal of improving quality of life for patients. In the private sector, this is done through a combination of medication and interventional procedures, while in the VA the focus is primarily on the latter. This is due to the VA system allocating the majority of medication management to primary care physicians. That’s not to say a VA pain physician will not provide suggestions for medication management when indicated, but they will not prescribe or manage this medication.
Within the VA system, pain management generally manages spinal conditions such as stenosis, non-surgical disc herniation, musculoskeletal trigger points, symptomatic spondylosis and unspecified radicular pain with absence of progressive neurological deficits. Sound familiar? Essentially, this department treats very similar conditions as chiropractors treat but with interventional procedures.
If you are like me at the beginning of my residency, you are currently asking, or have already Googled, what interventional procedures are. Interventional procedures include medial branch block, radiofrequency ablation, epidural steroid injection, sacroiliac (SI) joint corticosteroid injection and musculoskeletal trigger point corticosteroid injection. Intervention selection is determined by identifying the most likely pain generator and presence or absence of radicular symptoms. Below I have broken down each procedure into axial and radicular categories and provided a brief explanation of the goal.
Axial pain: symptomatic spondylosis, SI joint arthritis/dysfunction
Radicular: Disc herniation, Symptomatic spinal stenosis
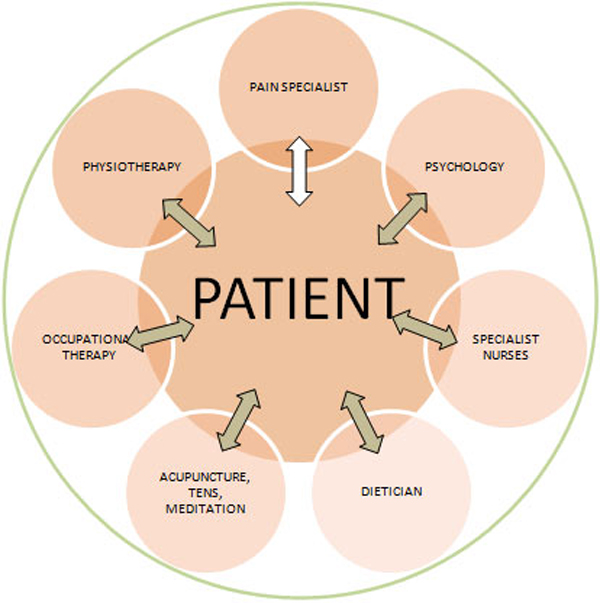
Unfortunately, we as chiropractors will also not be able to provide durable benefit to every person we see. There is a multitude of reasons this may happen, including lack of compliance to an active rehab program, sedentary lifestyle, co-morbidities and many others. Knowing when and where to refer an unresponsive patient is important. If a patient undergoes a reasonable trial of chiropractic care without having a decrease in pain, decrease in pain medication and/or increase in functional abilities, it is appropriate to seek other options. The next step may be physical therapy or acupuncture, but if the patient has already failed other conservative options, a next reasonable step is pain medicine. There may be some patients unwilling to consider injections, but it is your responsibility as a health provider to know the various options for care and when each is appropriate.
When choosing whom to refer to, it is important to research the physician to ensure you have the same ideals and goals. Explore options in the area by doing a quick search online or ask another health practitioner for referral options. Once two to five potential physicians have been identified, extend an invitation to coffee or lunch. Focus on learning more about the provider as a person, their practice approach and how working together can be mutually beneficial to improve patient outcomes. When in doubt, refer back to my alma mater’s (the University of Western States) motto: “for the good of the patient.” As practitioners, we are responsible to deliver care that aligns as such. This may not always be chiropractic care, and it’s important to be cognizant of the other options that are available in the extensive health care system.
Dr. Halloran is the chiropractic resident with the VA Connecticut Healthcare System under site director, Anthony Lisi, DC, and concurrently working towards her Master of Science in Human Nutrition and Functional Medicine through the University of Western States (UWS) as well as her diplomate in Diagnosis and Internal Disorders through the ACA. Dr. Halloran’s professional interests include advocacy and toxic exposure, nutritional deficiencies and chronic musculoskeletal pain within the veteran population.


Leave A Comment