A Model of Integrative Care for Low-back Pain
SOURCE: J Altern Complement Med. 2012 (Apr); 18 (4): 354–362
David M. Eisenberg, MD, Julie E. Buring, ScD, Andrea L. Hrbek, Roger B. Davis, ScD, Maureen T. Connelly, MD, Daniel C. Cherkin, PhD, Donald B. Levy, MD, Mark Cunningham, Bonnie O’Connor, PhD, and Diana E. Post, MD
Division of General Medicine and Primary Care,
Beth Israel Deaconess Medical Center,
Harvard Medical School,
Boston, MA 02115, USA.
OBJECTIVES: While previous studies focused on the effectiveness of individual complementary and alternative medical (CAM) therapies, the value of providing patients access to an integrated program involving multiple CAM and conventional therapies remains unknown. The objective of this study is to explore the feasibility and effects of a model of multidisciplinary integrative care for subacute low-back pain (LBP) in an academic teaching hospital.
DESIGN: This was a pilot randomized trial comparing an individualized program of integrative care (IC) plus usual care to usual care (UC) alone for adults with LBP.
SUBJECTS: Twenty (20) individuals with LPB of 3-12 weeks’ duration were recruited from an occupational health clinic and community health center.
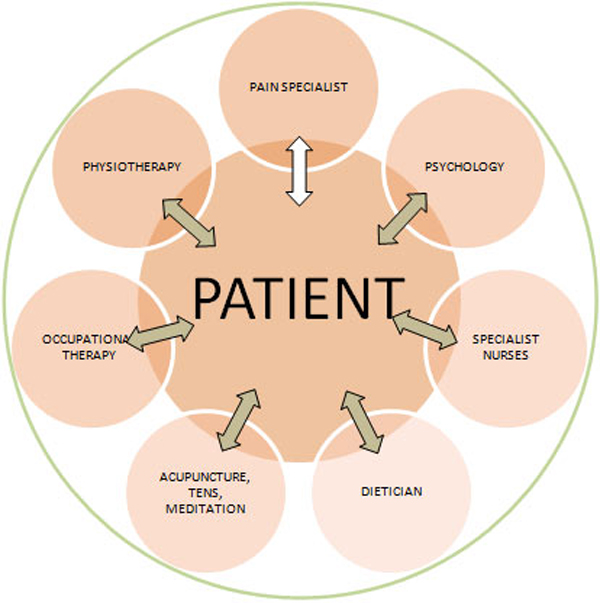
INTERVENTIONS: Participants were randomized to 12 weeks of individualized IC plus usual care versus UC alone. IC was provided by a trained multidisciplinary team offering CAM therapies and conventional medical care.
OUTCOME MEASURES: The outcome measures were symptoms (pain, bothersomeness), functional status (Roland-Morris score), SF-12, worry, and difficulty performing three self-selected activities.
RESULTS: Over 12 weeks, participants in the IC group had a median of 12.0 visits (range 5-25). IC participants experienced significantly greater improvements at 12 weeks than those receiving UC alone in symptom bothersomeness (p=0.02) and pain (p=0.005), and showed greater improvement in functional status (p=0.08). Rates of improvement were greater for patients in IC than UC in functional status (p=0.02), bothersomeness (p=0.002), and pain scores (p=0.001). Secondary outcomes of self-selected most challenging activity, worry, and the SF-12 also showed improvement in the IC group at 12 weeks. These differences persisted at 26 weeks, but were no longer statistically significant.
There are more articles like this @ our:
Integrated Health Care Page and the:
CONCLUSIONS: It was feasible for a multidisciplinary, outpatient IC team to deliver coordinated, individualized intervention to patients with subacute LBP. Results showed a promising trend for benefit of treating patients with persistent LBP with this IC model, and warrant evaluation in a full-scale study.
From the FULL TEXT Article:
Introduction
Four nationally representative surveys conducted between 1990 and 2007 demonstrated that a third or more of U.S. adults routinely use complementary and alternative medical (CAM) therapies to treat their principal medical conditions. [1–4] Total visits to CAM practitioners exceeded 300 million annually. [1, 2, 4] Total expenditures for CAM therapies were estimated at $14 billion in 1990, [1] $27 billion in 1997, [2] and $34 billion in 2007. [4] Out-of-pocket expenditures for CAM therapies in 2007 accounted for 11% of all out-of-pocket health care expenditures. [4] Despite the popularity of and substantial expenditures on CAM therapies, their effect on clinical outcomes and health care costs remains controversial. [5–8]
Low-back pain (LBP) is the most common medical condition for which adults use CAM therapies. [1, 2] BP is common, costly, and clinically challenging. An estimated 50% of adults experience significant LBP annually, and 70%—80% of adults are afflicted by LBP at some time in their lives. [9–11] In 1998, total health care expenditures incurred by individuals with LBP were estimated at $91 billion (1% of gross domestic product) with incremental expenditures attributable to back pain estimated at $26 billion. [12] These estimates excluded short- and long-term disability costs. Additional worker productivity losses due to pain-related conditions (with LBP as one of the three most costly) have been estimated at $61 billion per year. [13] In addition, wide variation in the medical and surgical management of LBP reflects widespread professional uncertainty about optimal care for this common condition. [14, 15]
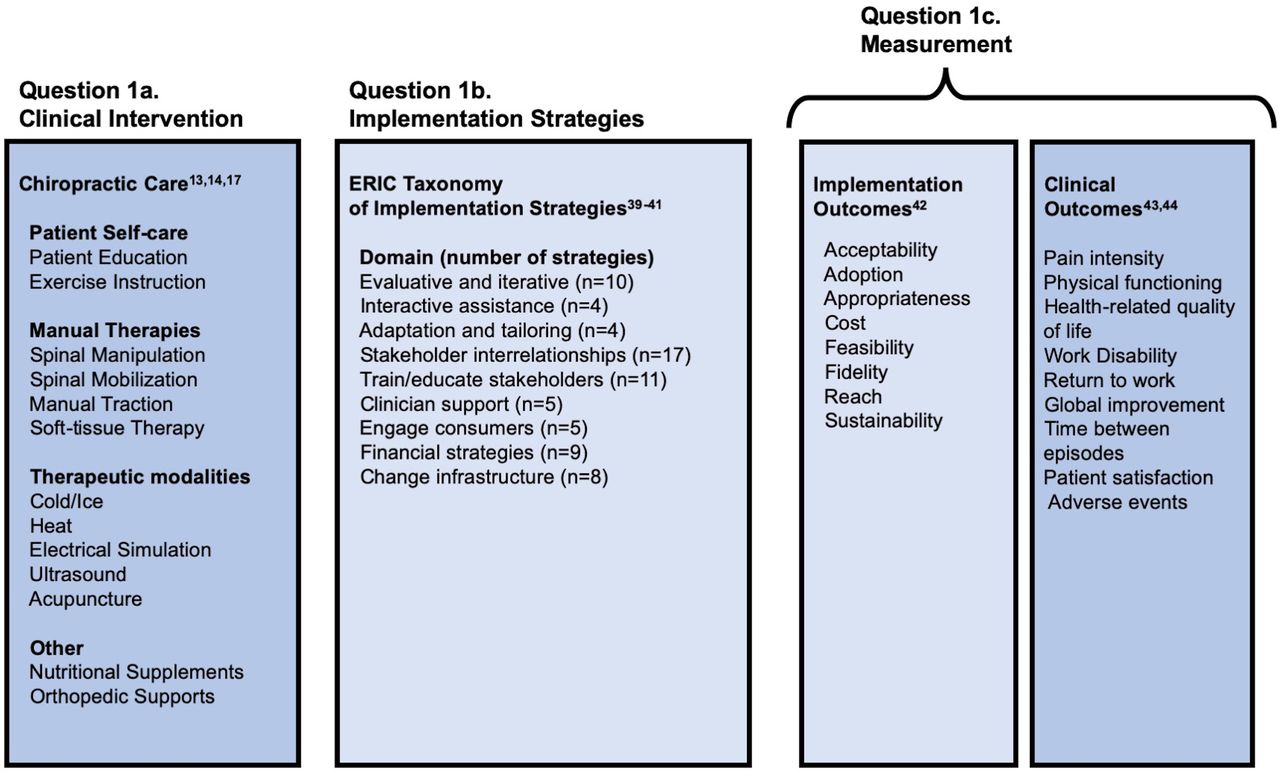
Among adults with LBP surveyed in 1997–1998, 59% saw both a medical doctor and used one or more CAM modalities. [2] In addition, nearly one third of all visits to CAM providers in 1997–1998 were made for the treatment of back or neck pain. [2, 16, 17] The evidence-based Clinical Guidelines jointly published by the American College of Physicians and the American Pain Society identified eight treatments for chronic LBP with “moderate” evidence of effectiveness (none had strong evidence), including four CAM therapies: acupuncture, massage, spinal manipulation, and yoga. [18]
However, these studies evaluated individual CAM modalities as opposed to multiple CAM (and conventional) modalities, as is commonplace in real-life settings. [19] Moreover, while other investigators have studied the effectiveness of various multidisciplinary approaches to the treatment of LBP, these have emphasized conventional medical and psychologic treatments with little or no use of CAM therapies as key components of their “integrative care teams.” [20–24]
To address this gap in knowledge, a pilot randomized trial was designed to explore the effectiveness of an individualized program of multidisciplinary, integrative care — which included CAM practitioners — plus usual care compared to usual care alone for adults with LBP. It is hypothesized that coordinated access to both conventional and CAM practices delivered by a team trained to provide individualized, multidisciplinary care will provide superior outcomes for patients with subacute LBP.
Read the rest of this Full Text article now!



Leave A Comment