AMI Model Working in Florida: Functional Improvements, Reduced Utilization Costs
by Medicaid Patients
SOURCE: Dynamic Chiropractic
Background: Alternative Medicine Integration (AMI) originally achieved recognition within the chiropractic community for its unique HMO model that utilized doctors of chiropractic as primary-care physicians (PCPs) and the portal of entry into an integrated health care delivery system, inclusive of hospitals, MDs and MD specialists and outpatient facilities. Contracted with Blue Cross Blue Shield’s HMO-Illinois, AMI’s integrated IPA demonstrated excellent clinical and cost outcomes.
These outcomes were published in the June 2007 issue of JMPT and reviewed in the June 4, 2007 issue of DC. [1] In July 2007, AMI received the national endorsement of the Congress of Chiropractic State Associations (COCSA) for its outcomes-based model of chiropractic medical management.
AMI also has been documenting the clinical and cost outcomes of its holistic, patient-centered disease management program for chronic pain patients enrolled in the Florida Medicaid system. While pharmaceutically oriented disease-management programs for diabetes, hypertension, COPD and heart disease have become staples of compliance-driven, cost-containment measures offered by insurance companies and managed-care organizations, largely unnoticed by media and consumers is the growth of costs associated with chronic pain, which has become the number-one cost driver for Medicaid and the commercial populations. Coupled with the national health care trend of increased pharmaceutical usage and its associated issues of prescription drug complications, contraindications, addiction to painkillers and accidental death inherent and measurable within the conventional medical model, treatment costs for chronic pain-related diagnoses continue to escalate.
AMI’s initial three-year findings suggest integrating complementary and alternative medicine with conventional care management approaches in the Florida Medicaid system reduces the cost of care for the payer and improves the quality of life for the patient. All indications point to the conclusion that an integrative approach to treating the “whole” person is effective in this patient population.
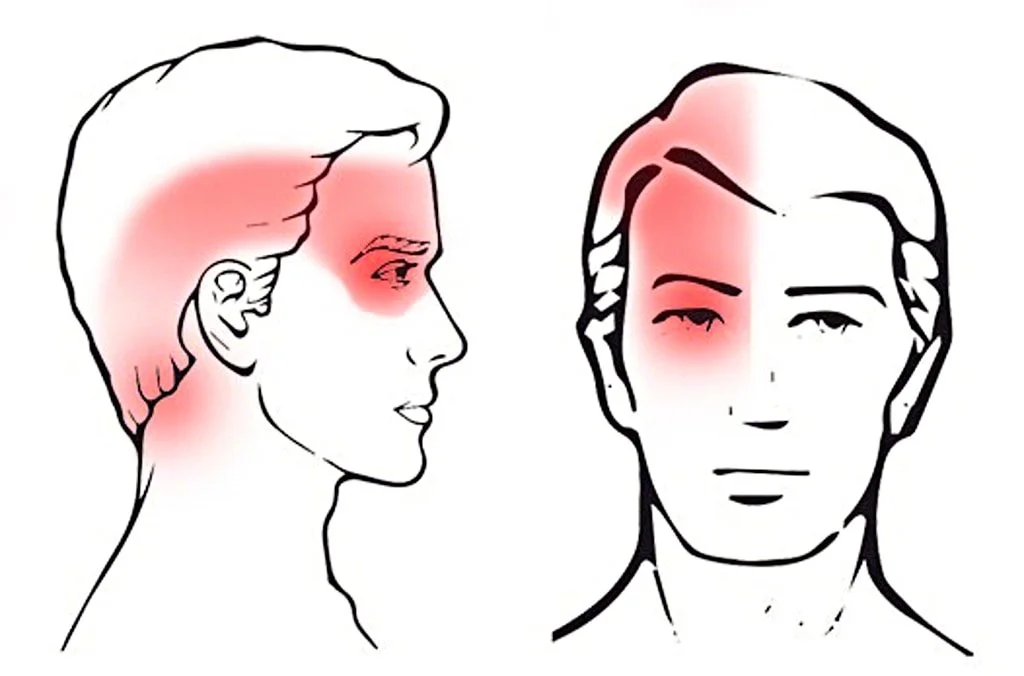
To chiropractors and other practitioners of natural medicine, this is not a surprise. Chances are you have anecdotal stories of patient improvement within this vulnerable and challenging population. However, what is noteworthy is that since April 2004, AMI has successfully worked with the state of Florida to provide services to those beneficiaries who have been diagnosed with chronic fatigue syndrome, chronic back pain, chronic neck pain and/or fibromyalgia. AMI’s holistic nurse case managers integrate the conventional medical care these beneficiaries receive with CAM services from providers including chiropractors, acupuncturists, massage therapists, nutritionists, pharmacists and registered nurse care managers.
There are more articles like this @ our:
Case managers refer appropriate patients to local chiropractors, much the same way they refer appropriate patients to local massage therapists or acupuncturists. In all cases, the case managers then coordinate information regarding the CAM therapies received back to the PCP. Enrolled beneficiaries also receive appropriate educational materials provided at the point of service, patient outreach phone calls, home visits, and access to community support groups.
Methods: Independent evaluators from the University of South Florida analyzed Medicaid claims data with dates of service from July 1, 2002 through June 30, 2005. Paid claims were analyzed for two distinct groups: an “eligible but not managed group” and an “eligible and managed group.” The former was comprised of 494 beneficiaries (11,446 case months) who received no CAM services during the study time frame. The latter group was comprised 185 beneficiaries (4,284 case months) who received CAM services during the same time frame.
Findings: Clinical improvement was measured utilizing the SF-12 to quantify changes in both mental and physical functioning. Compared to baseline, patients in the “eligible and managed group” averaged 20 percent improvement in both the physical and mental categories over a three-year period. This is noteworthy when compared with conventional pharmaceutically-oriented disease management programs, which rarely see improvements beyond 5 percent in either category. Ninety percent of the beneficiaries reported that “program treatment providers helped to reduce my levels of pain.”
Read the rest of this Full Text article now!



Leave A Comment