Current Trends in Chiropractic Research
An Interview with Malik Slosberg, DC
SOURCE: Health Insights Today ~ March 2014 ~ FULL TEXT
Interview by Daniel Redwood, DC
Malik Slosberg, DC, lectures throughout the United States and internationally. A professor at Life Chiropractic College West who has received many awards as an outstanding instructor, including “Teacher of the Year,” he has also served on the postgraduate faculty of ten chiropractic colleges and was named “Chiropractor of the Year” by the Parker Resource Foundation.
Dr. Slosberg has been in private practice for thirty years, has published numerous articles in chiropractic journals and is currently a columnist for Dynamic Chiropractic. In addition, he has produced educational materials including videos, wall charts, and patient handouts used by many chiropractic colleges and thousands of chiropractors worldwide.
Slosberg holds a Masters of Science degree from California State University in clinical counseling and a Physicians’ Assistant degree from Dartmouth College.
Those who attended Dr. Slosberg’s lecture at Cleveland Chiropractic College’s Homecoming in 2013 know that he is an excellent communicator with a strong grasp of chiropractic-related research. Along these lines, he has recently (1) given a presentation to the clinic directors of all of the chiropractic colleges in the world at the Association of Chiropractic Colleges 2013 meeting, on “Integrating Exercise Training in the Chiropractic Curriculum and Clinical Experience; (2) served as guest editor of a peer-reviewed Journal of Electromyography and Kinesiology special issue on spinal manipulation; and been the first chiropractor invited to be a guest faculty member at the Annual Integrative Holistic Medicine Conference.
Tell us about your background in chiropractic practice and teaching, and as an analyst and interpreter of chiropractic-related research?
Before I was a chiropractor, I was a physician’s assistant. I was trained at Dartmouth Medical School and practiced for three years with an internist-gastroenterologist who was chief of staff at the Naples, Florida hospital. Eventually, I just got sick of prescribing medications so I looked for an alternative that was more natural. Someone recommended chiropractic and I went to school without knowing much about chiropractic. After graduating, I started teaching a course titled “Subluxation Pathology.” I started reading a great deal of the peer-reviewed research, since I hadn’t really been exposed to the scientific literature as a student. Reading the data that was out there, I soon realized that this was information that chiropractors should really know. But I didn’t see that it was well disseminated. So I began to teach this course and then the seminars. I also had a chiropractic practice for just under 30 years. Throughout that time, I was always a faculty member at a chiropractic college, first at Life in Georgia and then at Life-West, out in California.
What do you consider the most significant current trends in chiropractic-related research?
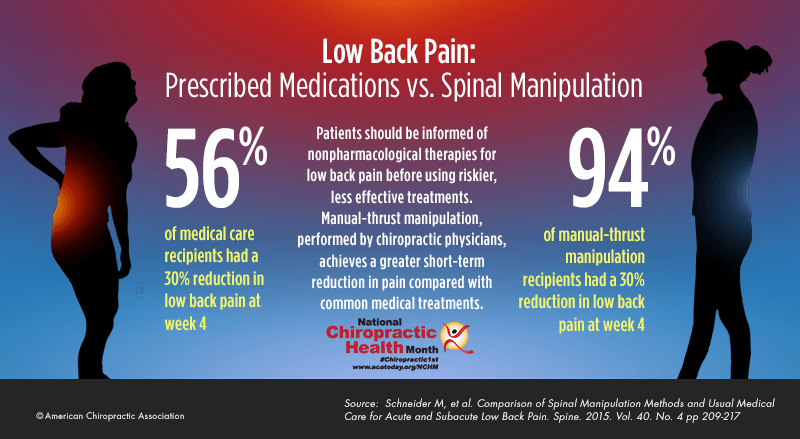
There are several that I think are quite significant. There are the recent high quality randomized trials evaluating the relative efficacy of chiropractic or spinal manipulation versus medical care, that is, versus anti-inflammatories, versus facet joint injections, and versus discectomies. This research has demonstrated that chiropractic is as effective or more effective, and often more cost-effective, than these more widely accepted medical interventions. This is important evidence and is being published in the areas of management of low back pain, neck pain, and also for headaches. Another area that I find really fascinating is the research on the impact of chiropractic on brain, including its influence on the sensory cortex, the motor cortex, and the cerebellum.
For so long, we talked about chiropractic reducing pressure on spinal nerves or, perhaps affecting alpha motor neurons in the spinal cord. But, we now we have more than 20 high-quality studies that confirm that chiropractic has rather profound effects on the central nervous system, particularly on motor control and on the processing somatosensory information.
Another area of great interest is chiropractic’s effect on the immune system. We have a number of recent studies consistently demonstrating that chiropractic adjustments reduce mediators of inflammation, that manipulation has anti-inflammatory effects. At the same time that adjustments reduce pro-inflammatory markers, they may also stimulate some of the immune regulatory cytokines to produce a more coordinated effect on infectious, invasive microorganisms. This evidence is still preliminary, and needs to be followed up by more studies.
In addition, two other areas of interest are the effect of chiropractic on general well-being, and enhancing chiropractic’s benefits when combined with rehab exercise. The systematic reviews document that if we combine chiropractic and rehab exercise, not only do we have more rapid pain relief but we also have significantly improved function and long-term improvement over multiple types of outcomes, when compared to spinal manipulation alone.
Those are a number of very important areas of study. Specifically with regard to the research on the effects of chiropractic care on overall well-being, how are those studies constructed?
For overall well-being, what has been investigated most are the effects on function, reducing disability, reducing pain, and improving quality of life. There is certainly a long road ahead for us in terms of improving the number and quality of these studies, but we definitely have at least preliminary evidence into the fact that chiropractic does indeed improve well-being, patient satisfaction, and global perceived effects. These are important patient-centered outcomes, highly regarded as evidence of effectiveness.
Looking at outcomes research, how would you characterize the current state of the science in terms of both musculoskeletal and non-musculoskeletal conditions? If a chiropractic student, for example, wants to summarize for a family member or someone in their community what has been demonstrated thus far by research, where would you suggest that they start?
I would say that high quality evidence consistently is supportive of the benefits of spinal manipulation and chiropractic care, for low back pain, for neck pain and for headache. That is where we have our strongest evidence.
The evidence on non-musculoskeletal conditions is much less substantiated. We have a number of scattered studies looking at conditions from enuresis to otitis media, but there is not really a coherent database for the non-neuromusculoskeletal effects of manipulation. The studies I mentioned earlier about the immune system are evolving into a sound database, but the others are not quite there yet. In addition, funding for nonmusculoskeletal research has not been there. It is an area that, hopefully, will be very fertile in the future, but right now it really lacks a sound foundation. I don’t think at this point that we should be promoting that chiropractic is effective for some of these non-musculoskeletal conditions.
You’re among the leading chiropractic lecturers on cutting edge developments in mechanism-related research, including studies on the effects of chiropractic adjustments on the brain and other neural structures. Tell us more about these developments. You lectured on this last year at Cleveland Chiropractic College.
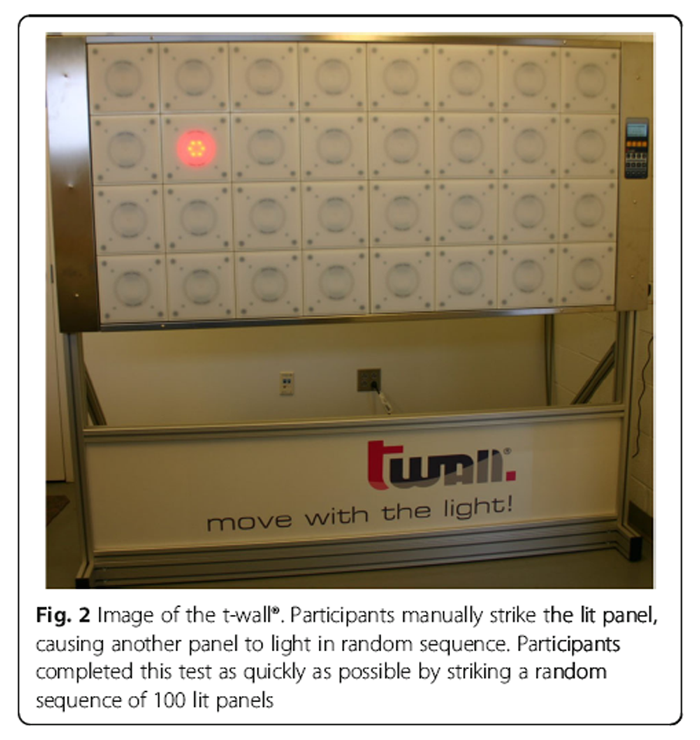
This is an enormously fertile area of research, spearheaded by two women, Bernardette Murphy and Heidi Haavik, who are both chiropractors as well as PhD neurophysiologists. Between the two of them, they have about 20 studies demonstrating the effectiveness of manipulation on various aspects of central nervous system and brain function.
Some of the things that have been demonstrated by them, as well as other researchers, are that chiropractic affects glucose utilization in the brain, that chiropractic affects perfusion of blood to the brain, that chiropractic affects oxygen saturation of the blood in the brain, that chiropractic increases excitability of inhibited muscles (which we know occur in chronic back pain, for example), and that chiropractic specifically can excite corticomotor neurons that drive muscles to protect, stabilize and move the spine. Those are the areas I find most exciting. There is a progressive accumulation of research on all of above functions.
With glucose utilization in the brain, or oxygen saturation levels, in what ways might those findings translate, sooner or later, into either improved patient care or better understanding of the effects of chiropractic adjustments. I’m asking about applicability.
Many of these findings are more abstract in their contribution to the science of how chiropractic affects the brain. In terms of practical application, what we are starting to see is that adjustments improve neuromotor control by affecting brain function and that they improve the pattern of coordination, coactivation, recruitment and sequencing of muscles, to provide dynamic stability throughout a full range of motion with good load distribution, and minimize undue stresses and strains on various tissues. As this occurs, of course, this helps normalize joint function and it normalizes sensory input, changing dysafferented or garbled input into more normal input. It also improves the brain’s ability to process that input and design more effective motor control. So overall, we have less disability, improved function, an improved sense of well-being and movement patterns.
As you mentioned earlier, in recent years there has been a significantly increased emphasis on the role of exercise, both in research and in chiropractic practice. How important is it that chiropractors include exercise in case management, rather than strictly limiting their interventions to manual methods?
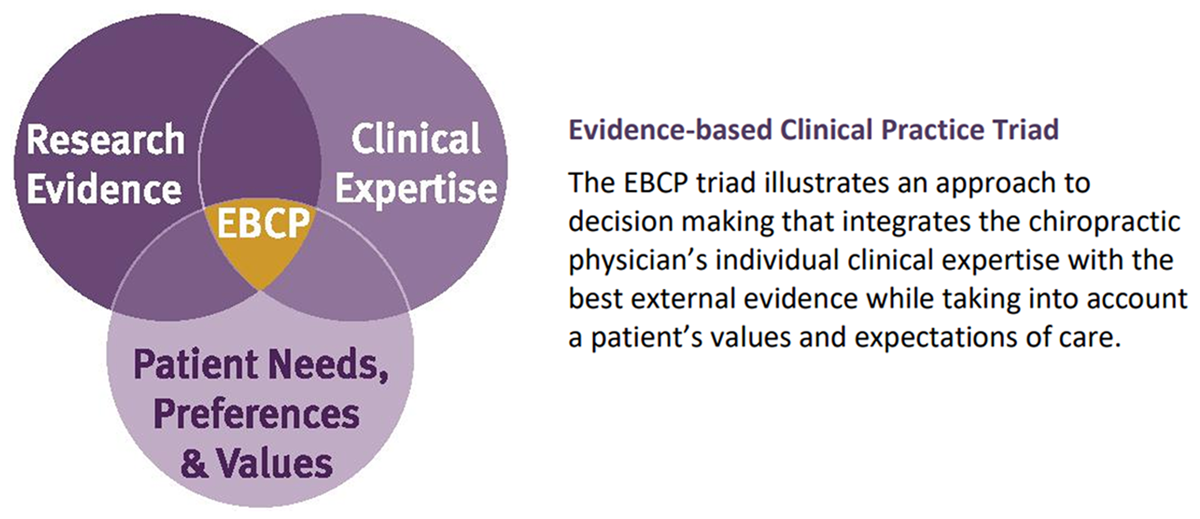
Chiropractic is an applied clinical science, which means that it continually evolves as the research grows and methods of application, of techniques to improve patient well-being and function change to incorporate the new insights and evidence. So as the database changes, the clinical application has to change in accordance with the research.
Research has been evolving for a long time, particularly in the last ten years, to demonstrate how effective exercise is at improving function, well-being, quality of life, as well as, cognitive function. We now have now quite a few studies—including major systematic reviews of the literature—that demonstrate that if we incorporate exercise into chiropractic care, not only do we minimize recurrences, but we also have improved short- and long-term benefits over a broad spectrum of outcomes, compared to what we would see if we did manipulation alone.
Other studies indicate improved satisfaction when exercise is incorporated into patient management. And critically, it gets the patient engaged as an active participant of the team to restore and maintain his or her health. That’s really essential. The Council on Chiropractic Guidelines and Practice Parameters (CCGPP) in 2008 stated that the ultimate goal of chiropractic is to improve patients’ function and help them regain responsibility for their health. So exercise is the primary form of active care, in which the responsibility is placed on the patient, and the chiropractor is not just the adjustor but the patient’s coach. Together they work to improve the patient’s health and help the patient gain a sense of responsibility and control.
I remember in your presentation at Cleveland last year, you showed some scans comparing muscular development and strength in people who exercise regularly versus those who don’t. I’m also recalling that you yourself are an exercise enthusiast.
Yes, I am. I try to practice what I read, and what I preach. There’s really an abundance of very recent literature that demonstrates significant benefits from exercise, and particularly exercise involving high-intensity types of activity, when the metabolic demand is very high. It appears that the body, and particularly the nervous and muscular systems, requires regular metabolic challenges in order to gain and maintain optimal function. So exercise has multiple effects. We generally think of it as being effective for motor function, but we’ve come to realize through recent research that it has profoundly beneficial effects on the brain: improving glucose utilization, reducing insulin resistance, improving cognitive function and memory, improving mood, and actually enlarging the size of the hippocampus, which is critical for emotional regulation, as well as, memory and learning. Exercise has benefits for all kinds of other dimensions of neurologic and higher brain function that had never been correlated with exercise until recently. The evidence on these benefits is very exciting, as are the mechanisms of how they occur.
With regard to mental health, we had a lecture here a few years ago by James Gordon, MD, who is board certified in psychiatry and chaired the White House Commission on Complementary and Alternative Medicine Policy. Among other things, he made the case that there is actually stronger evidence for the benefits of exercise in treating depression than for antidepressant drugs, if you take into account all of the clinical trials, including the ones that the drug companies suppressed but which later emerged as a result of various lawsuits.
I’ve also been reading a great deal lately about the effects of exercise for post-traumatic stress disorder, dementias, depression and bipolar disease. Inactivity and a sedentary lifestyle, combined with a typical American diet that is high in refined carbs, sugars and omega-6 fats all contribute to a decline of major regions of the brain, particularly the dorsolateral prefrontal cortex and the hippocampus.
We know that shrinking of the hippocampus occurs with Alzheimer’s, vascular dementias, and depression. It also occurs with bipolar disease and posttraumatic stress disorder. The damage to the hippocampus seems to be the major factor in cognitive decline and mood. Several recent studies show that exercise can markedly increase the size of the hippocampus. In a 2010 study on spinning classes, in which participants attended 30-minute sessions three times a week, healthy subjects increased the cross-sectional area of the hippocampus by 16 percent in just three months.
An emphasis on exercise is central to chiropractic practice and to the natural health worldview that has always been part of chiropractic.
Right, it’s a key part of a healthy lifestyle that encourages activity, physical well-being and optimal function. And what we know today is that activity must be included in order to have optimal function.
Given finite limits to funding of research related to chiropractic, what would you suggest regarding the types of research that should be prioritized now and in the coming years?
We have a lot of studies on chiropractic and low back pain. We have a lot of studies on chiropractic and neck pain. We have an increasing number of studies on chiropractic for managing headaches. In the future, we really need to pursue more about the effects of chiropractic on the central nervous system and its effects on physical well-being, and brain and motor function. I think these are areas of great importance which will open the door to diverse and holistic effects of chiropractic care in combination with an active, healthy lifestyle.
We also need more research on chiropractic and the immune system, not only with regard to its anti-inflammatory effects but also in terms of the ways the nervous system and the immune system now appear to be part of an integrated single system involved in recognizing and fighting infections and other challenges to the body. All of these are areas that I think will further validate the value of chiropractic in the future and will also be exciting to patients.
Daniel Redwood, DC, the interviewer, is a Professor at Cleveland Chiropractic College–Kansas City. He is the editor-in-chief of Health Insights Today, associate editor of Topics in Integrative Healthcare and serves on the American Chiropractic Association’s editorial advisory board. Dr. Redwood’s website and health policy blog are at www.redwoodhealthspeak.com.

Leave A Comment