Chronic Low-Back Pain: Is Infection a Common Cause?
SOURCE: ACA News ~ September 2013
By Daniel Redwood, DC
Background:
A 2013 randomized trial by Hanne Albert and colleagues at the University of Southern Denmark, published in the European Spine Journal, [1] found that 100 days of treatment with a disc-penetrating antibiotic was significantly more effective than a placebo for relief of chronic low-back pain (CLBP) in people whose MRI exam showed Modic Type 1 changes, which are associated with degeneration and inflammation. If confirmed by other studies, this would mean that disc infection is a far more common cause of CLBP than previously known.
Rare indeed is the publication of a Research paper with the potential to overturn long-standing, fundamental assumptions about the nature of a disease. Virtually all clinical research is incremental in its expansion of our knowledge — by evaluating the effectiveness of treatment methods, demonstrating the conditions under which they are most likely to be beneficial and exploring the physical mechanisms through which they work. But every now and then, a study like Marshall and Warren’s 1982 discovery [2] of the association between the heliobacter pylori bacterium and peptic ulcers appears out of left field to upend what previously passed for conventional wisdom.
In recent years, arguably the only publication to trigger a major reorientation of our understanding in an area critical to chiropractic practice was the 2008 Cassidy et al. paper in Spine, [3] in which the investigators examined nine years of medical records in the Canadian province of Ontario (covering 100 million patient years) and were able to definitively demonstrate that the likelihood of a stroke is no greater if one visits a doctor of chiropractic (DC) than if one visits a medical doctor. Overnight, this study shifted our understanding of stroke vis-à-vis chiropractic, with the authors concluding: “The increased risks of VBA (vertebrobasilar artery) stroke associated with chiropractic and PCP (primary care physician) visits is likely due to patients with headache and neck pain from VBA dissection seeking care before their stroke. We found no evidence of excess risk of VBA stroke associated (with) chiropractic care compared to primary care.”
There’s a lot more material like this @:
Is the Albert et al. study on antibiotics treatment of CLBP this kind of game-changer?
New Evidence on Infection and Low Back Pain:
Must We Change Our Perspective?
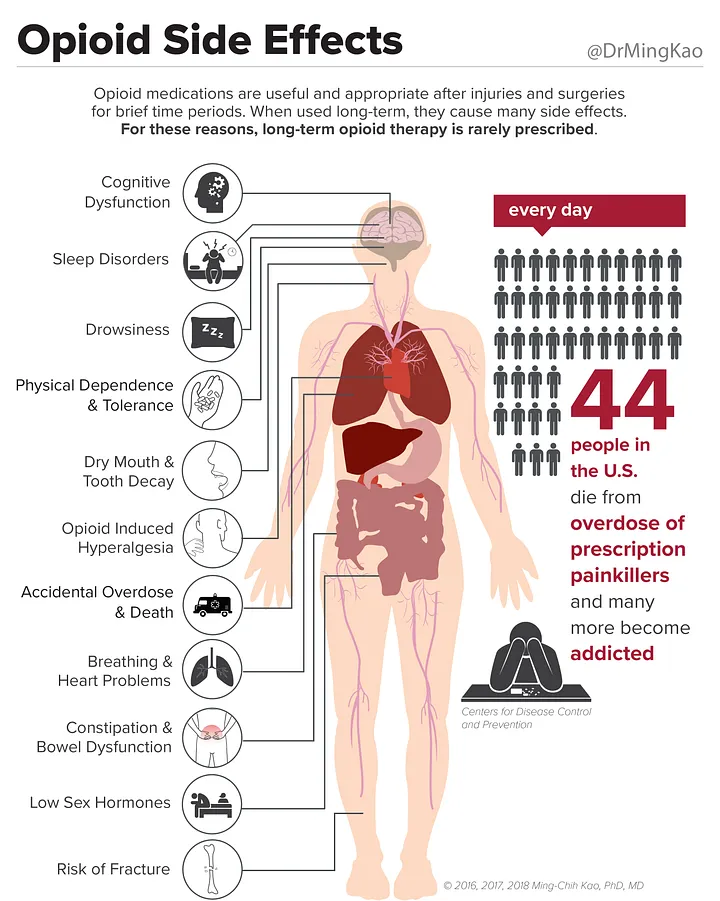
Generations of DCs have been taught that infection, malignancy and fracture are “red flag” conditions that require referral for medical care. Until now, low-back pain identified as having an infectious etiology has been a rare enough occurrence that a doctor of chiropractic might go for years without seeing such a case.
This widespread view on the rarity of infection as a cause of CLBP — held by DCs and medical professionals alike — is sharply challenged by two 2013 papers [1, 4] in the European Spine Journal by Hanne Albert and colleagues at the University of Southern Denmark. Their work builds on previous studies, including one involving 247 people in which nuclear material taken from the intervertebral discs of people with lumbar disc herniations and other spinal disorders such as scoliosis, fracture and tumors was examined, and bacteria (i.e., primarily the anaerobic organism P. acnes) were present in 37 percent of cases involving disc herniation and 0 percent of non-disc cases. [5]
Albert’s group sought to determine whether previously nonresponsive CLBP with Modic Type 1 changes on MRI would respond to antibiotic therapy. The researchers’ European Spine Journal trial [1] clearly indicates that the answer is yes. But unlike the several-day course of antibiotics typically recommended for a bacterial infection of the upper respiratory tract, these intra-disc infections appear to require a much longer course of antibiotic therapy — 100 days in the Albert et al. study.
SIDEBAR:
Read the rest of this Full Text article now!



I can hear the scalpers now:
Come on Down!
This stuff is
Better than Placebo!
Whooooeee!
Great post, so informative. Thanks for sharing!
Hi
I recently suffered a slipped disc and sciatica which turned out to be the most painful experience of my life, no exaggeration!.
I’ve tried just about everything possible to ease the pain and nothing seems to be working.
In my desperation I did a Google search for another solution and I came across a treatment called Inversion Therapy. I had never heard of this before and I wondered what your thoughts were on this as a treatment, can this genuinely help people with a prolapse disc?
I found the information about inversion therapy on The British Back Institute’s Website, they seem to have some good advice on the site, so would like to hear what you guys think.
Thanks
Joe
Hi Joe
Talk about a can-o-worms!
All this “therapy” provides is traction. A recent study (http://www.ncbi.nlm.nih.gov/pubmed/222636480) did find some benefit…BUT they only followed these 10 individuals for 6 weeks.
Avoiding surgery is wonderful, and a recent worker’s compensation study showed that you are almost 300% more likely to return to work if you DO NOT get surgery. [1]
Please do not misunderstand…traction, all by itself appears to be helpful, but unless it is also coupled with education (ala the McKenzie approach) about avoiding prolonged flexion at the waist (leaning forwards in a chair etc) [2] then it’s really only a matter of time before these same individuals will end up with new, or recurrent disc complaints.
1. New Study Reveals That Back Surgery Fails 74% of the Time
SPINE (Phila Pa 1976) 2011 (Feb 15); 36 (4): 320–331
2. Body Alignment, Posture, and Gait
Chapter 4 from: “Clinical Biomechanics: Musculoskeletal Actions and Reactions”