Outcomes of Usual Chiropractic; Harm (OUCH) Randomised Controlled Trial of Adverse Events
SOURCE: Spine 2013 (Sep 15); 38 (20): 1723-9 ~ FULL TEXT
Walker, Bruce F. DC, MPH, DrPH; Hebert, Jeffrey J. DC, PhD;
Stomski, Norman J. BHSc (hons), PhD; Clarke
Murdoch University School of Engineering and Information Technology,
Mathematics & Statistics,
Murdoch University Centre for Health,
Exercise and Sports Medicine,
University of Melbourne.
Study Design. Blinded parallel-group randomized controlled trial.
Objective. Establish the frequency and severity of adverse effects from short-term usual chiropractic treatment of the spine when compared with a sham treatment group.
Summary of Background Data. Previous studies have demonstrated that adverse events occur during chiropractic treatment. However, as a result of design limitations in previous studies, particularly the lack of sham-controlled randomized trials, understanding of these adverse events and their relation with chiropractic treatment is suboptimal.
Methods. We conducted a trial to examine the occurrence of adverse events resulting from chiropractic treatment. It was conducted across 12 chiropractic clinics in Perth, Western Australia. The participants comprised 183 adults, aged 20 to 85 years, with spinal pain. Ninety-two participants received individualized care consistent with the chiropractors’ usual treatment approach; 91 participants received a sham intervention. Each participant received 2 treatments.
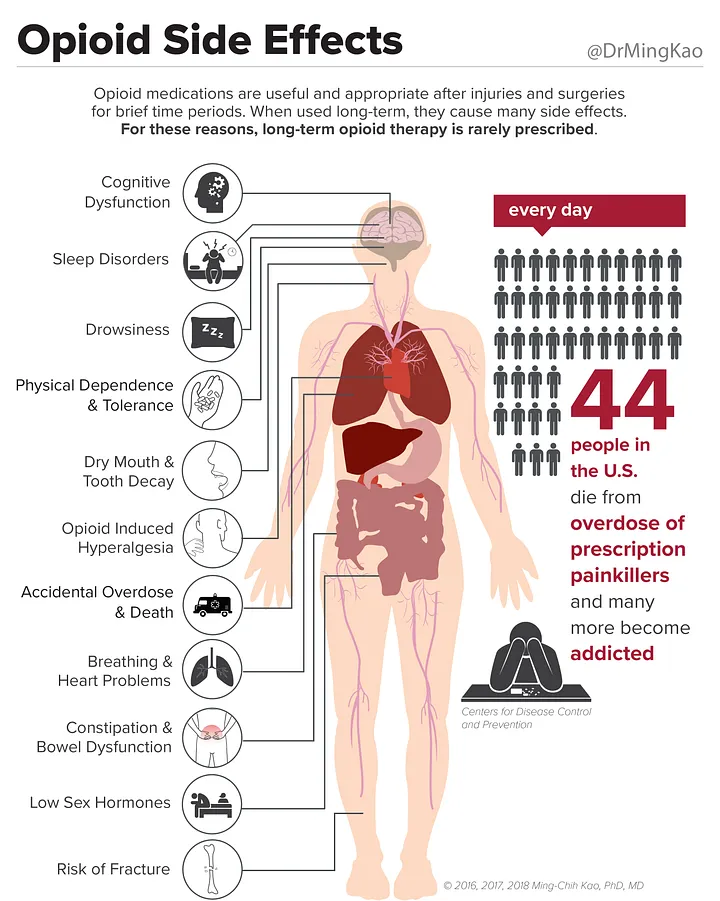
Results. Completed adverse questionnaires were returned by 94.5% of the participants after appointment 1 and 91.3% after appointment 2. Thirty-three percent of the sham group and 42% of the usual care group reported at least 1 adverse event. Common adverse events were:
increased pain (sham 29%; usual care 36%),
muscle stiffness (sham 29%; usual care 37%),
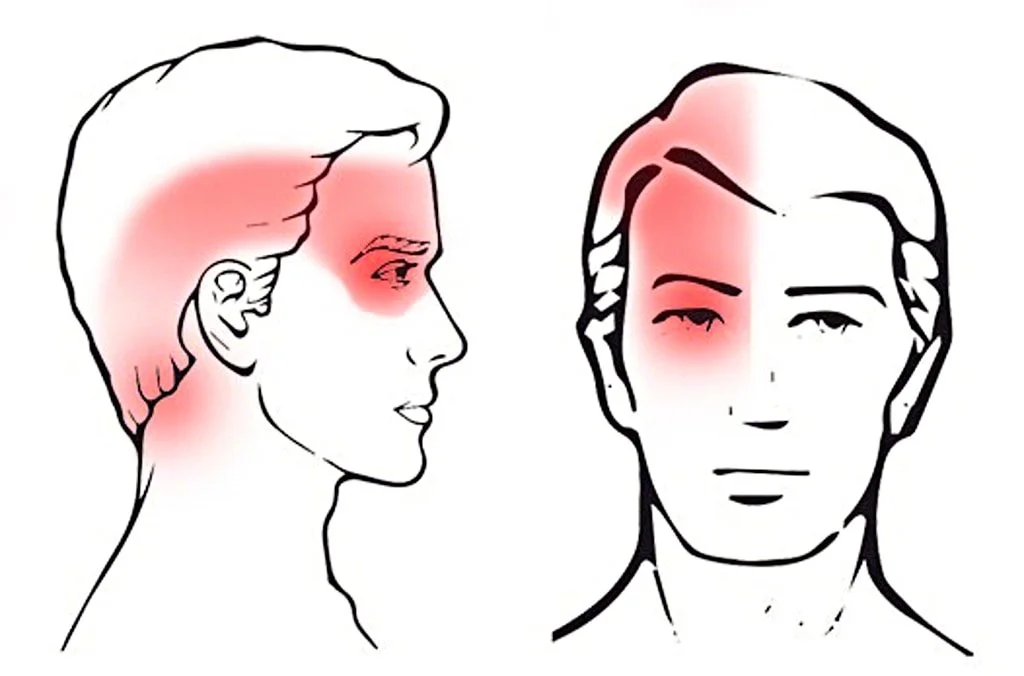
and headache (sham 17%; usual care 9%).
The relative risk (RR) was not significant for adverse event occurrence (RR = 1.24; 95% CI: 0.85–1.81),
occurrence of severe adverse events (RR = 1.9; 95% CI: 0.98–3.99),
adverse event onset (RR = 0.16; 95% CI: 0.02–1.34),
or adverse event duration (RR = 1.13; 95% CI: 0.59–2.18).
No serious adverse events were reported.
Conclusion. A substantial proportion of (previously reported) adverse events following chiropractic treatment appear to result from natural history variation and nonspecific effects.
From the FULL TEXT Article
Introduction
Chiropractic therapy is commonly used to manage musculoskeletal conditions in high-income countries. [1, 2] The occurrence of adverse events resulting from chiropractic treatment is of considerable interest to chiropractors and the general public. Most adverse events associated with chiropractic treatment are mild, short lasting, and typical of musculoskeletal condition symptoms. [3–11] However, due to a lack of appropriately designed studies, particularly sham-controlled trials, there are differences in views about what constitutes a chiropractic treatment–related adverse event.
The occurrence of adverse events after chiropractic treatment has been examined in 1 randomized controlled trial, [3] 5 prospective single-arm studies, [4–8] and 3 retrospective studies. [9–11] These studies reported that 34% to 61% of participants experienced at least 1 adverse event. [4–8] Most events were benign, transient, and typically consisted of increased pain, muscle stiffness, tiredness, headache, and radiating discomfort. [4–8] Less common events were dizziness, nausea, tinnitus, and impaired vision. More serious adverse events associated with chiropractic treatment, including disc injury, cauda equina syndrome, fracture, and stroke, have been reported but the rate has not been robustly established. [9, 11–13]
Predictors of adverse events have been identified in 4 previous studies of chiropractic treatment. [6–8, 14] These predictors included female sex, [6, 8] age (27–46 yr), [14] high-velocity manipulation (compared with low-velocity mobilization), [14] first treatment session, [6] medication use, [14] more than 1 region treated or only thoracic spine treated, and [14] treatment including cervical rotation, [8] work status, [8] and general practitioner visit in previous 6 months. [8] Notably, none of the identified predictors have been found to influence adverse events consistently across studies.
Several limitations constrain the findings of previous studies. In the prospective studies, the chiropractors providing treatment also administered the questionnaires, which possibly resulted in underreporting of adverse events. [4–8] In addition, recall bias may also have led to an underestimation of adverse events in the retrospective studies. [15]
Moreover, all previous studies lacked a sham intervention, which may have resulted in an overestimation of adverse events, as some events could have been associated either with natural history or with nonspecific effects. Therefore, the estimates of adverse events resulting from the specific effect of treatment are not known. What is known is that adverse events after chiropractic treatment of spinal pain range from trivial to catastrophic. Given these facts, plus the limitations of previous studies, additional research is required to develop a more accurate safety profile of chiropractic treatment.
We assessed whether common adverse events differed between participants who received usual chiropractic treatment or a sham intervention for spinal pain. We also captured information about the types, severity, onset, and duration of adverse events.
Intervention Components
Each participant was assigned to either a sham group or a usual chiropractic group, whereupon 2 treatments were delivered with approximately 1 week between treatments. The chiropractors delivering either the sham or usual chiropractic treatment attended a training session that provided instruction about the trial and how to undertake their respective treatments. To be eligible, all chiropractors need to practice within the Western Australian metropolitan region and were required to be registered with the Chiropractic Board of Australia.
Sham group: the practitioners in this group comprised 4 registered chiropractors who administered at each visit
(c) a randomly placed hand on the spine while ultrasound was administered to give a “hands-on” experience.
Usual care: the practitioners in this group consisted of 8 registered chiropractors who provided individualized chiropractic care consistent with their usual treatment approach. The only condition that may have influenced the chiropractors’ usual treatment approach was a request to adhere to Australian imaging guidelines. [21]
DISCUSSION
This was the first study to use a sham-controlled design to examine adverse events after chiropractic treatment.
A substantial proportion of adverse events experienced during chiropractic care for spinal pain may be the result of natural symptom fluctuation or from nonspecific effects. Adverse events were common in both the usual chiropractic care and sham groups, but no important differences were seen between the groups and no serious adverse events were reported. However, although very similar, the estimates of severe adverse event risk arising from the intention to treat and available case analyses resulted in conflicting conclusions. Although the intention-to-treat approach was our primary analysis, we cannot rule out the possibility of increased risk of severe adverse event occurrence with chiropractic treatment compared with sham therapy. The adverse event rate reported by the usual care group in this study was consistent with rates reported by previous studies (42% compared with 34%–61%). [4–8]
Moreover, the finding that most adverse events were benign and transitory is also consistent with other chiropractic studies. [4–8] The proportion of adverse events in these previous studies due to other effects such as natural history or nonspecific effects remains indeterminable because none of the studies used a sham arm. However, the results of our study suggest that many adverse events experienced after chiropractic treatment result from either natural history variation or nonspecific effects. Some may view these results as evidence that chiropractic treatment is essentially an entirely benign intervention, but it more likely reflects that our study was underpowered to detect a statistically significant difference between groups.
Studies of interventions other than manual therapies have also associated nonspecific effects with adverse events. [24–26] Interestingly, some studies demonstrated that the adverse events reported by participants in either the placebo or the sham arm mirror the adverse events in the active intervention arm. [27–31]
This association has been attributed in part to the effect of patient expectancy, which typically depends on details about possible adverse events conveyed through information sheets, consent forms, or the investigators’ behavior. [24–31] Other studies have shown that a strong aversion to experience an adverse event, coupled with a sense of helplessness about avoiding it, may evoke negative emotions and subsequent reductions in beneficial nonspecific effects. [32] It then seems likely that an expectation of adverse events coupled with not wanting to experience adverse events may promote nonspecific effects that contribute to adverse events. [32]
Careful consideration should be given to how the information from this study is presented to patients. As numerous studies have shown, disclosing information about the risks of adverse events increases the likelihood of adverse events occurring. [24–31] Conversely, framing information about adverse events in positive terms (noting that most patients did not experience an adverse event), rather than negative terms (detailing the minority who experienced an adverse event), can lead to a lower adverse event rate. [33, 34] In light of this, we recommend that a form of words be developed for chiropractic patients that accurately reflects the results of our study about potential common adverse events without unnecessarily engendering fear.
Conducting this study under typical clinical conditions enhances the external validity of our findings. However, this study was powered to detect a 20% difference in adverse events; therefore, we were underpowered to detect the magnitude of between-group differences observed in our sample of participants. In terms of internal validity, we did not measure either anxiety or depression, and it should be noted that it is possible that differing levels of anxiety or depression may have influenced the participants’ experience of adverse events in either group. However, there were no important differences between groups in the psychosocial characteristics we assessed at baseline including the Pain Catastrophizing Scale and Fear-Avoidance Beliefs Questionnaire. Nevertheless, it should be noted that it is possible that differing levels of anxiety or depression may have influenced the participants’ experience of adverse events in either group.
We endeavored to blind study participants to group allocation but were unsuccessful. This was probably due to inherent difficulties in finding an adequate sham intervention to use in a chiropractic trial or indeed any type of randomized controlled trial. [35] The lack of blinding success may have influenced the reporting of adverse events. In particular, the adverse event rate may have been underreported in the sham group as the majority thought they were receiving an inactive intervention.
Finally, the chiropractors providing usual care were more experienced than chiropractors delivering the sham intervention. However, experience is unlikely to affect an inert sham intervention such as that delivered in this trial. It may be the case that the more experienced chiropractors had better interpersonal skills, which may have reduced the number of adverse events attributable to nonspecific effects.
CONCLUSION
Additional studies of larger and more diverse populations are warranted. Such studies should be powered to detect the magnitude of between-group differences observed in this trial and include a wait list arm to account for natural variation in spinal pain.


It is also important to consider which types of chiropractic care were used to minimize any inconsistent results.
Montgomery County Chiropractic Center
Hi Dr. Conrad
The full text defines the care provided, however it’s usually safe to conclude that it was diversified technique, since that is taught at virtually every college.
The studies that use non-traditional techniques, from instrument adjusting to NUCCA to Gonstead always mention the technique by name, to distinguish it from diversified.
I understand Palmer College is currently comparing 3 different techniques for lowering blood pressure. That should raise some eyebrows.
I find it interesting that of the sham group 33% reported at least one adverse event, this from de-tuned ultrasound, an Activator tuned to zero and random ‘hands-on’ therapy. And they experienced more headaches post-treatment than the treatment group. The study goes on to conclude, “It then seems likely that an expectation of adverse events coupled with not wanting to experience adverse events may promote nonspecific effects that contribute to adverse events.” Some entangled meaning in that statement for others to mull over.
Hi John: Actually, there’s a term for that: The Nocebo Effect, the evil twin of placebo. I like the authors suggestion to de-emphasize minimal events, to avoid a self-fulfilling prophecy.
How much care did they follow in this study?
1 visit, 1 week, 1 month?
Dr. Schotzko
This study involved 2 visits, with the intention of measuring the quantity and quality of reported short-term *adverse* events. So, if you were asking whether they were followed-up for a long period of time, I’m not clear what the value of that would be.
Previous studies have noted that some percentage of individuals report such events EARLY ON in their care program, and we have all seen it in our practices. Safety studies have also shown that the occurrance of severe reactions is so small that it would most likely take a study with millions of participants to track them, and that’s never going to happen. That is why most studies of stroke incidence have been retrospective file reviews.
The value of this study is twofold: First, it indicates that some of those complaints may have occurred even without care (natural history), and second that we might reduce the nocebo effect by how we explain things to our patients at the beginning of care.