Sports Management: Shoulder Girdle Injuries
We would all like to thank Dr. Richard C. Schafer, DC, PhD, FICC for his lifetime commitment to the profession. In the future we will continue to add materials from RC’s copyrighted books for your use.
This is Chapter 22 from RC’s best-selling book:
“Chiropractic Management of Sports and Recreational Injuries”
Second Edition ~ Wiliams & Wilkins
These materials are provided as a service to our profession. There is no charge for individuals to copy and file these materials. However, they cannot be sold or used in any group or commercial venture without written permission from ACAPress.
Chapter 22: Shoulder Girdle Injuries
This chapter concerns injuries of and about the scapula, clavicle, and shoulder. In sports, the shoulder girdle is a common site of minor injury and a not infrequent site of serious disability. It is second only to the knee as a chronic site of prolonged disability. Upper limb injuries amount to about 20% of sport-related injuries. They can be highly debilitating, require considerable lost field time, and can easily ruin a promising sports career.
Introduction
The versatile shoulder girdle consists of the sternoclavicular, acromioclavicular, and glenohumeral joints, and the scapulothoracic articulation. These allow, as a whole, universal mobility by way of a shallow glenoid fossa, the joint capsule, and the suspension muscles and ligaments. The shoulder, a ball-and-socket joint, is freely movable and lacks a close connection between its articular surfaces.
The regional anatomy offers little to resist violent shoulder depression, and the shoulder tip itself has little protection from trauma. The length of the arm presents a long lever with a large head within a relatively small joint. This allows a great range of motion with little stability. The stability of the shoulder is derived entirely from its surrounding soft tissues.
History and Initial Care
A careful history recording the mechanism of trauma and the position of the limb during injury, careful inspection and palpation of the entire region, muscle and range-of-motion tests, and other standard neurologic-orthopedic tests will often arrive at an accurate diagnosis without the necessity of x-ray exposure. Forceful manipulations should always be reserved for late in the examination to evaluate contraindications.
Contusions, strains, sprains, bursitis, and neurologic deficits must be alertly recognized and treated. Fractures and dislocations, obviously, take precedence over soft-tissue injuries with the exception of severe bleeding. Always check for bony crepitus, fracture line tenderness and swelling, angulation and deformity. Because the shoulder readily “freezes” after injury, treatment must strive to maintain motion as soon as possible without encouraging recurring problems. The key to avoiding prolonged disability is early recognition and early mobilization.
There are more materials like this @ our:
Posttraumatic Assessment
As in any musculoskeletal disorder, evaluation should include muscle strength grading, joint ranges of motion, sensory perception, appropriate tendon reflexes, and various other clinical tests (eg, laboratory, roentgenography), depending upon the situation at hand. A review of pertinent neurologic, orthopedic, and peripheral vascular manuevers, reflexes, and tests relative to the shoulder girdle and arm is shown in Table 22.1.
Referred Pain
As the shoulder lies between the neck and the hand, pain from the neck or distal upper extremity may be referred to the shoulder, and a shoulder disorder may refer pain to the neck or hand. In shoulder disorders, differentiation must include cervical problems, superior pulmonary sulcus tumor, and referred pain from viscera. Pain can also be referred to the shoulder by brachial plexus involvement, pectoralis minor syndrome, anterior scalene syndrome, claviculocostal syndrome, suprascapular nerve entrapment, dorsal scapular nerve entrapment, cervical rib, spinal cord tumor, arteriosclerotic occlusion and other vascular disorders.
The origin of shoulder pain may be a viscerospinal reflex such as seen in some diaphragmatic, gallbladder, aortic, pleural, and coronary diseases. If you are able to reproduce pain during joint motion, the condition is most likely neuromuscular in origin. Pain that cannot be reproduced points towards a visceral origin.
In cases of a herniated cervical disc (common at C5-6), pain may radiate from the neck into the arm, forearm, hand. The head and neck will be deviated to the affected side with marked restriction of movement. The shoulder will usually be elevated on the same side with the arm slightly flexed at the elbow (protective position). Biceps and triceps reflexes will be lost or diminished. Paresthesias and sensory loss in the dermatome distribution will be found corresponding to the disc involved.
Myofascial Shoulder Syndromes
In most cases of posttraumatic shoulder pain, its origin can generally be localized to a small area by palpation or reproduced at some point in active or passive motion. This is typical of many common disorders — capsulitis, bicipital tendinitis, dislocations, impingement syndromes, rotator cuff strains, subacromial bursitis, and supraspinatus injuries, for example.
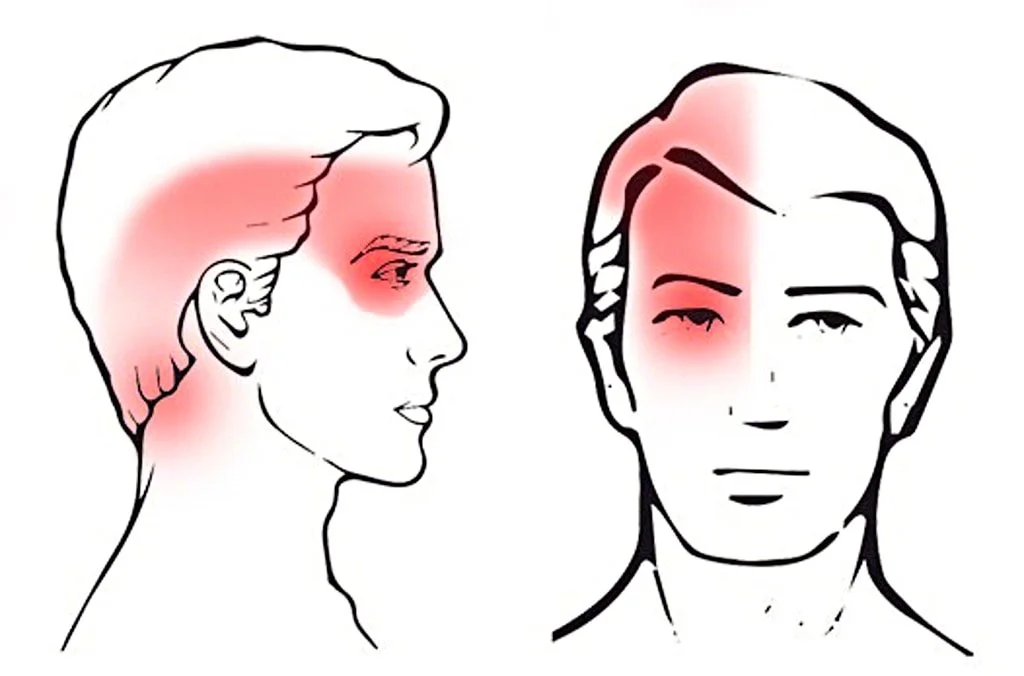
Trigger point pain differs from that associated with most structural injur- ies in that the physical findings are few. Rather than being localized, the pain is described over a broad area that do not coincide with specific segmental patterns. Associated paresthesiae are described in extremely vague expressions. Range of motion tests and muscle strength grading offer little help, even after referred pain from the cervical spine, lungs, or viscera is ruled out. While trauma may be involved, it may be only a precipitating rather than a causative factor.
The muscles of the shoulder girdle are highly susceptible to trigger point formation because they are anatomically susceptible to fatigue, easy victims of the stresses of poor posture and biomechanical faults, and the target for many psychosomatic reflexes. Michele/Eisenberg state that no less that one-third of their middle-aged patients with shoulder pain had the myofascial pain syndrome.
The focal point of pain in a myofascial syndrome will be found as one or more small areas of muscle fiber degeneration that feel fairly firm and ropey to the touch. Further probbing will usually elicit the characteristic involuntary “jump sign” as the patient reacts and the physiologic “twitch sign.” This latter sign is the result of a brief contraction of the surface fibers near the trigger point.
Although a trigger point may develop in any muscle, certain sites appear to be favorite locations. A point in the superior medial aspect of the scapula, near the insertion of the levator scapulae, is a common site, as are points in the supraspinatus and trapezius. Weed describes frequently occurring points over the heads of the 2nd, 3rd, or 4th ribs, just lateral to the spinous processes.
Management. As in other areas, goading, acupuncture, high-volt stimulation, spray-and-stretch, and deep percussion/vibration are generally the conservative therapies of choice in trigger point therapy.
Sensitive Trigger Points
| Review the complete Chapter (including sketches and Tables) at the ACAPress website |



Leave A Comment