Predictors of Outcome in Neck Pain Patients Undergoing Chiropractic Care: Comparison of Acute and Chronic Patients
SOURCE: Chiropractic & Manual Therapies 2012 (Aug 24); 20 (1): 27
Cynthia K Peterson, Jennifer Bolton, B. Kim Humphreys
University of Zürich and Orthopaedic University Hospital Balgrist, Forchstrasse 340, 8008 Zürich, Switzerland
Background Neck pain is a common complaint in patients presenting for chiropractic treatment. The few studies on predictors for improvement in patients while undergoing treatment identify duration of symptoms, neck stiffness and number of previous episodes as the strong predictor variables. The purpose of this study is to continue the research for predictors of a positive outcome in neck pain patients undergoing chiropractic treatment.
Methods Acute (< 4 weeks) (n = 274) and chronic (> 3 months) (n = 255) neck pain patients with no chiropractic or manual therapy in the prior 3 months were included. Patients completed the numerical pain rating scale (NRS) and Bournemouth questionnaire (BQ) at baseline prior to treatment. At 1 week, 1 month and 3 months after start of treatment the NRS and BQ were completed along with the Patient Global Impression of Change (PGIC) scale. Demographic information was provided by the clinician. Improvement at each of the follow up points was categorized using the PGIC. Multivariate regression analyses were done to determine significant independent predictors of improvement.
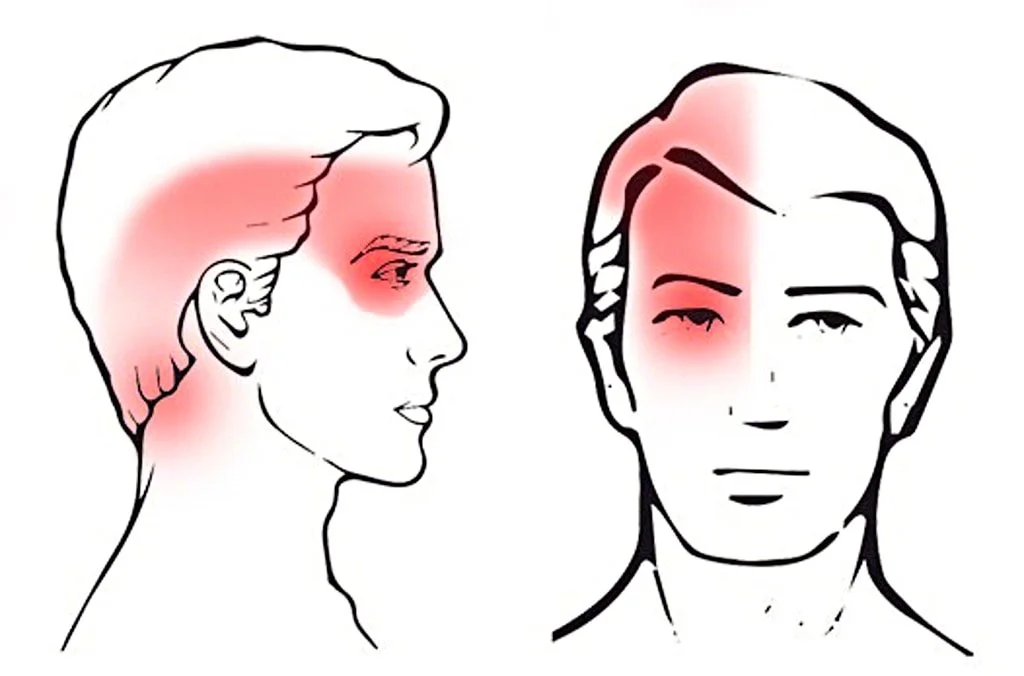
Results Baseline mean neck pain and total disability scores were significantly (p < 0.001and p < 0.008 respectively) higher in acute patients. Both groups reported significant improvement at all data collection time points, but was significantly larger for acute patients. The PGIC score at 1 week (OR = 3.35, 95% CI = 1.13-9.92) and the baseline to 1 month BQ total change score (OR = 1.07, 95% CI = 1.03-1.11) were identified as independent predictors of improvement at 3 months for acute patients. Chronic patients who reported improvement on the PGIC at 1 month were more likely to be improved at 3 months (OR = 6.04, 95% CI = 2.76-13.69). The presence of cervical radiculopathy or dizziness was not predictive of a negative outcome in these patients.
CONCLUSIONS: The most consistent predictor of clinically relevant improvement at both 1 and 3 months after the start of chiropractic treatment for both acute and chronic patients is if they report improvement early in the course of treatment. The co-existence of either radiculopathy or dizziness however do not imply poorer prognosis in these patients.
There are more articles like this @ our:
From the FULL TEXT Article:
Background
Patients suffering from neck pain are second only to low back pain patients in terms of the frequency of presentation for chiropractic treatment [1-4]. For many of these patients the precise diagnosis is difficult to ascertain and thus becomes labeled ‘non-specific’ neck pain or neck pain from mechanical dysfunction [1,3-5]. Research evidence has yet to determine with clarity whether spinal manipulative therapy (SMT) or mobilization of the neck is the superior treatment for these patients [1-9] although it appears that both of these treatments have better outcomes when combined with exercise [5,10].
Manipulative therapy to the cervical spine has traditionally been considered somewhat controversial by certain health care practitioners. Recent high quality research evidence supports the relative safety of chiropractic SMT to the cervical spine with no increased risk of vertebral artery injury compared to patients seeking care from other primary medical physicians who do not manipulate the neck [11-13]. A few studies have begun to investigate specific predictors for a positive response to chiropractic SMT in neck pain patients and have identified the duration of symptoms, stiffness of the neck and the number of previous episodes of neck pain as some of the strongest predictors of an immediate positive response [7,8,14]. Therefore, the purpose of this study is to continue the research for predictors of positive outcomes in neck pain patients undergoing chiropractic treatment and to determine if these differ between acute and chronic patients.
DISCUSSION
The predictors of improvement in acute and chronic neck pain patients undergoing chiropractic treatment appear to be very similar to those found for patients suffering from low back pain [18-25]. The most consistent predictor of improvement for both acute and chronic neck pain patients was reported prior improvement. Acute patients who reported being improved 1 week after the start of treatment were approximately 3 times more likely to be improved at 3 months while chronic neck pain patients who reported being improved at 1 month were over 6 times more likely to also report improvement at 3 months.
Although the various demographic details collected at baseline in this study were largely not predictive of improvement at 1 week, 1 month or 3 months, it is important to emphasize two clinical conditions that were not predictive of a worse outcome. Thus neck pain patients who also had cervical radiculopathy (34 acute and 29 chronic patients) or who reported associated dizziness (51 acute and 64 chronic patients) improved as much as neck pain patients without these additional signs or symptoms. Previous studies on low back pain patients undergoing chiropractic treatment reported that the presence of additional leg pain was a negative predictor of improvement [25-27]. The Swiss chiropractors contributing patients to this current study were specifically informed prior to the start of data collection that the presence of arm pain alone was not sufficient to diagnose radiculopathy and that clinical signs of nerve root compression were also required. However, it was left up to the individual chiropractor to make this diagnosis based on clinical experience. There was no attempt to determine whether or not their diagnosis was correct. Swiss chiropractors have a significant amount of exposure to patients with radiculopathy in their mandatory two year post-graduate program and were therefore assumed competent in their diagnosis.
Acute neck pain sufferers (symptoms < 4 weeks) presented with higher levels of pain and disability compared to chronic patients (symptoms > 12 weeks), but improved more quickly and in a higher proportion than chronic patients. Although the acute patients did better than the chronic patients (in part due to the natural history of neck pain), it is important to point out that many of the chronic patients also improved. Additionally, the percentage of chronic patients reporting improvement continued to rise at each data collection time point whereas this appeared to level off at 1 month for acute patients. This study intentionally analyzed acute and chronic patients separately rather than including duration of neck pain into the prediction model. Previous research has already shown that duration of neck pain is a strong predictor of outcome [7] and it was particularly desired to assess the outcomes of chronic patients as they are the ones who are often more challenging and expensive to treat. Although there was no significant age difference between the acute and chronic neck pain patients in this study, the chronic patients were significantly less likely to be in paid employment, reported significantly more prior episodes of neck pain and were less likely to be in good general health. The duration of symptoms and the number of previous episodes of neck pain have been found to be predictors of outcome in previous studies [7,8,14]. Surprisingly, this study did not find that the number of previous episodes of neck pain was linked with improvement as reported by Rubinstein et al. [7]. However, there was a difference between the Rubinstein et al. study and this current study in the way previous neck pain episodes were classified. This variable was dichotomized (yes/no) in the Rubenstien et al. study compared to categorizing previous episodes into one of three groups (none, 1–3, 4 or more) in this current study. It was hoped that providing more specific detail about the number of previous episodes would prove to be predictive of improvement. However, this was not the case. Also as reported in other studies, the majority of patients in this study were women, particularly in the chronic category [1,3]. This may be one reason why chronic patients were less likely to be in paid employment. Women, particularly with children, are less likely to work outside of the home in Switzerland compared to some other western countries [28].
Limitations
There are several limitations to this study. Although a high proportion of both acute and chronic neck pain patients improved at all time points, without a control group this improvement cannot be attributed to treatment. It is also acknowledged that the improvement for many of the acute patients was most likely due to natural history. In this study we collected baseline variables using paper questionnaires but subsequent outcomes were collected through telephone interviews. It has been shown that telephone interview data may have a slightly positive effect on outcomes encouraging patients to report more favorably [29-31]. An attempt was made to minimize this effect by employing anonymous research assistants, unknown to the patients, who collected the telephone data from the university rather than from the practice setting where the patient was being treated.
Data was also purposely not collected on specific treatments applied or frequency of chiropractic treatment. It would be interesting and important for the education of chiropractors to compare treatment and technique methods with patient outcomes in the future. Data was collected in this study on the date of the last treatment however, and this will be evaluated and reported when the 1 year outcomes data is assessed in the near future.
Another limitation to the study may be the validity of the Bournemouth Questionnaire to adequately measure the psychosocial domains such as depression, anxiety, etc. as these variables were not predictive of improvement at 3 months. However, when compared to the NPAD and NDI the BQ was much more sensitive to change on all domains [16], including the domains of anxiety, depression, fear avoidance and pain locus of control. Certainly ‘depression’ was identified as a negative predictor of improvement at 1 month in the multivariate analysis for acute patients which suggests that for depression, at least, the BQN is sensitive as a predictor of outcome.
A further limitation may be the fact that most of the variables that were not continuous variables were dichotomized into yes/no or present/absent with the exception of ‘number of previous episodes’ and ‘general health’. This was done to facilitate the clinical utility of this study and assist in interpretation of the results. In most cases there was a straightforward yes/no (i.e. smoking, paid employment, etc.) answer. In those few variables where this was not the case, we used clinical experience to make the decision and it is fair to say that we may have made the wrong judgment on those two variables which were categorized with three options. This is the same model used in a similar research study done on low back pain patients however [18].
Although this study found that neither the presence of radiculopathy nor dizziness were negative predictors of outcome, no power analysis was done to determine whether the 115 patients with dizziness or the 63 patients with radiculopathy were adequate sample sizes to definitively draw these conclusions. However, at least for the dizziness patients, 115 is approximately one fifth of the total sample of 529 patients.
Previous research has identified ‘stiffness’ as a predictor of outcome (8) in neck pain patients treated with SMT. This was not included in the baseline evaluations done by the treating chiropractors and is therefore another limitation in this study.
The final possible limitation to this study may be the fact that compared to baseline there were fewer patients at the 1 and 3 month analyses. This was primarily due to the fact that it was not yet time for the 1 month and 3 month telephone calls for several patients. However, both the acute and chronic groups at 3 months had nearly 200 patients each. The first author of this study is directly in charge of large medical databases in two departments at this hospital. Experience of periodically calculating and monitoring pain scores, PGIC scores, proportions of patients improving or worsening with various treatments in these databases has NVconsistently demonstrated that once a threshold of approximately 100 patients in a cohort is reached, additional patients make minimal difference in the statistical results calculated. Therefore this missing data is unlikely to have changed the outcomes with sample sizes this large. If outcome data was available for any of the follow-up time periods, the patient and their baseline data remained in this study.
CONCLUSIONS:
For the most part, baseline variables were not predictive of outcome in neck pain patients and as a consequence prediction of outcome at 1 week was not possible using the potential predictors measured in this study. Instead, the most consistent predictor of improvement at both 1 and 3 months for both acute and chronic neck pain patients undergoing chiropractic treatment is significant self-reported improvement early on. Importantly, the co-existence of cervical radiculopathy or dizziness in addition to neck pain was not associated with a negative outcome for either acute or chronic patients.




Interesting study. It was neck and arm pain that caused me to become a chiropractor. When I have a patient that complains of a “hot poker” in their arm I can relate. After receiving medications that allowed my problem to progress it was suggested I see a chiropractor. Within a few weeks I was without pain. I think many of the older chiropractors have similar stories to tell. It would be intersting to compare outcome assessments between medical and chiropractic under the same roof.