TMJ Trauma and Its Rehabilitation
Clinical Monograph 13
By R. C. Schafer, DC, PhD, FICC
TEMPOROMANDIBULAR JOINT DYSFUNCTION
Proper treatment of TMJ dysfunction must be based on a thorough case history, a complete physical workup, an evaluation of the cranial respiratory impulse and craniosacral mechanisms, and a detailed examination of the TMJ, cranium, and cervical spine. Unfortunately, radiographs to determine abnormal joint space are rarely successful unless over 30% of the bone has been destroyed.
A blow to the jaw is easily transmitted to the temporal bones. As mentioned previously, osteopathic research suggests that a subluxated temporal bone is often the focal fault. This is reported to be grossly indicated by flattening (temporal internal rotation) or protrusion (temporal external rotation) of an ear from the skull.
Symptomatology
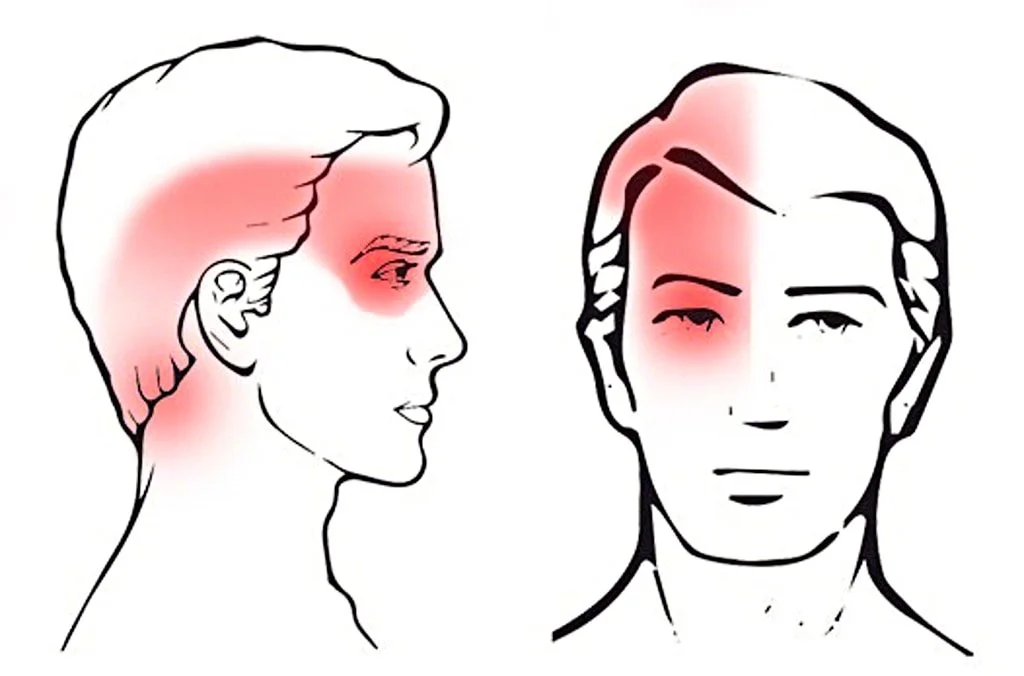
The major symptoms of TMJ dysfunction are masticator muscle fatigue and pain, which are usually described as a severe, unilateral (rarely bilateral), dull facial ache that is often fairly localized to an area just anterior to the tragus of the ear. The onset of pain is gradual, progressively increasing over several days or months. It is aggravated by chewing and opening and closing the mouth. Precipitation is often made by eating an apple, a wide yawn, snorkeling, prolonged dental work, playing a wind instrument, prolonged chewing, a bump or pressure on the mandible, sleeping in the prone position, or a cervical whiplash.
You may also enjoy our page on:
Joint clicking, popping, or grinding are often felt and/or heard with or without auscultation. The mandible deviates to one side when opened, tenderness and muscle spasm are present, and a nervous bruxism is usually in the history. There is pain on opening and closing the mouth, or, sometimes, just by moving the head on the neck. An associated referred earache is common, but it should be noted that an ear disorder can sometimes refer pain to the TMJ area.
Neurologic and Circulatory Effects. Nine of the 12 cranial nerves are in close relation to the temporal bones from which the mandible is suspended; thus, universal effects may be expressed. There is no doubt that TMJ dysfunction can have far-reaching effects, even to the point of involving peripheral circulation and paresthesias. S. D. Smith reported a case where major improvement in leg circulation directly corresponded to balancing a left TMJ compression through jaw repositioning.
Referred Pain. Within the immediate area of the TMJ are found the chorda tympanum nerve and branches of the superficial temporary artery, vein, and nerve wherein area irritation may cause reflex pain in other areas. While pain is often referred from the TMJ to the scalp, supraorbital area, ear, or neck, the TMJ is rarely a site of referred pain except in cases of a tooth abscess in the mandible or an inflamed upper or lower wisdom tooth impaction.
Differentiation should first be made from angina or cardiac infarction, both of which often refer pain, aching, or throbbing to the angle and base of the mandible. Sinusitis usually refers pain to the frontal area, but sometimes pain is referred to the jaw. Temporal arteritis and glaucoma can also refer pain to the jaw. Referred pain may also be due to dental pathology such as dental caries, pulpitis, impaction, occlusal trauma, periapical abscess, and cementitis. Referred pain from a lower molar is carried by the trigeminal, which also supplies the external pterygoid muscle.
Associated Spasticity. The location of associated muscle spasm in TMJ dysfunction according to incidence is in the external pterygoid, internal pterygoid, masseter, posterior cervical, temporalis, sternomastoideus, trapezius, and mylohyoid. Rhomboid and scalene attachments to the first rib are also commonly tender and hypertonic.
Inspection and Palpation
Active joint motion is observed by having the patient open and close the mouth, observing the movement of the mandible from the front and sides. The rhythm should be smooth, the arc should be continuous and unbroken, and the mandible should open and close in a straight line symmetrically, with the teeth easily separating and joining. An awkward arc, a restricted range of motion, and/or lateral deviation during motion suggest an abnormality.
Read the rest of this Full Text article now!
Enjoy the rest of Dr. Schafer’s Monographs at:



Having worked with the dental profession over the past 30 years has afforded me the opportunity to work with many dentists. One of the most important diagnostic considerations facing doctors who consider treatment of TMJ symptoms and causes of the cranio-facial dysfunction patients is the differential diagnosis between temporomandibular joint disorder and cervical dysfunction.
Dr. Stephen D. Smith, doctor of dental medicine, states: “An assessment of the cervical pain and headache is basic to manual manipulative medicine, musculoskeletal evaluation and/or chiropractic medicine and physical therapy assessments. Palpatory examination offers both objective as well as subjective aspects of information on the patient related to pain and potential referral patterns in the head region. Cervical range of motion is also essential, particularly in establishing a baseline at initial evaluation concerning fixation of vertebrae, muscle spasm areas of somatic contracture and other neck related patterns, all of which can affect the jaw muscles an TMJ apparatus when evaluating TMJ symptoms and causes.” Chiropractors are positioned to play a critical role in the management of TMD.
Does anyone have any video on the adjustment techniques?
You may find some online, but it’s certainly preferable to learn ANY manual technique face-to-face, with lots of feedback.
@Marco: I may be a little biased, but I would get Dr. Leonard Faye’s DVD’s on Motion palpation and adjustive procedures. There’s 2 DVD’s with the TMJ section on the 2nd DVD. I found the DVD’s to be well made and worth every penny. And more important, my patient’s have benefitted greatly with this approach.