Cervical Spine Trauma
We would all like to thank Dr. Richard C. Schafer, DC, PhD, FICC for his lifetime commitment to the profession. In the future we will continue to add materials from RC’s copyrighted books for your use.
This is Chapter 4 from RC’s best-selling book:
“Chiropractic Posttraumatic Rehabilitation”
These materials are provided as a service to our profession. There is no charge for individuals to copy and file these materials. However, they cannot be sold or used in any group or commercial venture without written permission from ACAPress.
CHAPTER 4: CERVICAL SPINE TRAUMA
The cervical spine provides musculoskeletal stability and supports for the cranium, and a flexible and protective column for movement, balance adaptation, and housing of the spinal cord and vertebral artery. It also allows for directional orientation of the eyes and ears. Nowhere in the spine is the relationship between the osseous structures and the surrounding neurologic and vascular beds as intimate or subject to disturbance as it is in the cervical region.
BACKGROUND
Whether induced by trauma or not, cervical subluxation syndromes may be reflected in total body habitus. IVF insults and the effects of articular fixations can manifest throughout the motor, sensory, and autonomic nervous systems. Many peripheral nerve symptoms in the shoulder, arm, and hand will find their origin in the cervical spine, as may numerous brainstem disorders.
COMMON INJURIES AND DISORDERS OF THE CERVICAL SPINE
Cervical spine injuries can be classified as
(1) mild (eg, contusions, strains);
(2) moderate (eg, subluxations, sprains, occult fractures, nerve contusions, neurapraxias);
(3) severe (eg, axonotmesis, dislocation, stable fracture without neurologic deficit); and
(4) dangerous (eg, unstable fracture-dislocation, spinal cord or nerve root injury).
Spasm of the sternocleidomastoideus and trapezius can be due to strain or irritation of the sensory fibers of the spinal accessory nerve as they exit with the C2—C4 spinal nerves. The C1 and C2 nerves are especially vulnerable because they do not have the protection of an IVF. Radicular symptoms are rarely evident unless an IVD protrusion or herniation is present.
PREVALENCE
Because of its great mobility and relatively small structures, the cervical spine is the most frequent site of severe spinal nerve injury and subluxations. A large variety of cervical contusions, Grade 1—3 strains and sprains, subluxations, disc syndromes, dislocations, and fractures will be seen as the result of trauma.
The most vulnerable segments to injury are the axis and C5—C6 according to accident statistics. Surprisingly, the atlas is the least involved of all cervical vertebrae. In terms of segmental structure, the vertebral arch (50%), vertebral body (30%), and IVD (30%) are most commonly involved in severe cervical trauma. While the anterior ligaments are only involved in 2% of injuries, the posterior ligaments are involved in 16% of injuries.
EMERGENCY CARE
In the emergency-care situation, the patient with spinal cord injury must be treated as if the spinal column were fractured, even when there is no external evidence. Immediate and obvious symptom of spinal cord injury parallel those of fractures of the spinal column. The establishment of an adequate airway takes priority over all other concerns except for spurting hemorrhage.
In general, trauma anteriorly to the neck implies soft-tissue damage and possible airway obstruction; trauma posteriorly suggests cervical spine and cord damage; and lateral trauma indicates possible vascular and musculature damage. Due to relative head weight to neck strength and other anatomic differences, neck injury is more critical in the very young.
INITIAL ASSESSMENT
If there are no severe complaints or recognizable signs of major disability, ask the patient to conduct mild active movements if able to do so without discomfort. If slight straight axial compression on top of the head produces unilateral or bilateral radiating root pain, deep injury must be suspected and precautions taken immediately. After the neck has been evaluated, check possible injury to other parts of the body.
Knee and ankle reflexes can be tested, but the neck should not be moved. Stabilize the neck before assessment of severity. A collapsed patient should never be asked to sit or stand until major disability has been ruled out. The first point in analysis is knowing the mechanism of injury. Without moving the patient, check vital signs and palpate for swelling, deep tenderness, deformity, and throat cartilage stability. When logical, another person should apply gentle bilateral traction on the cervical area via the skull during palpation.
Are there bleeding, spasm, pain, motion restrictions, sensory changes, signs of shock? Limb weakness or dysesthesia indicates nerve root compression. Injuries of the upper airway or alimentary canal feature ventilation abnormalities, stridor, bubbling wound, subcutaneous emphysema, hoarseness and dysphagia, bloody sputum, nosebleed, bloody vomitus, or unexplained wound tenderness. Injuries to the cervical nerves are suggested by deviation of the tongue, drooping mouth corner, sensory deficits, and Horner’s syndrome. Cervical fractures are commonly associated with severe pain, spasm, and joint stiffness. Vascular injuries feature vigorous bleeding, absent superficial artery pulsations, an enlarging or pulsatile hematoma, and stroke signs. If there is any suggestion of injury to the carotid artery, palpation should be avoided. Such an injury should be suspected if there is a diagonal erythematous contusion on the side of the neck. Palpation may encourage complete carotid occlusion.
POSTTRAUMATIC ROENTGENOGRAPHIC CLUES
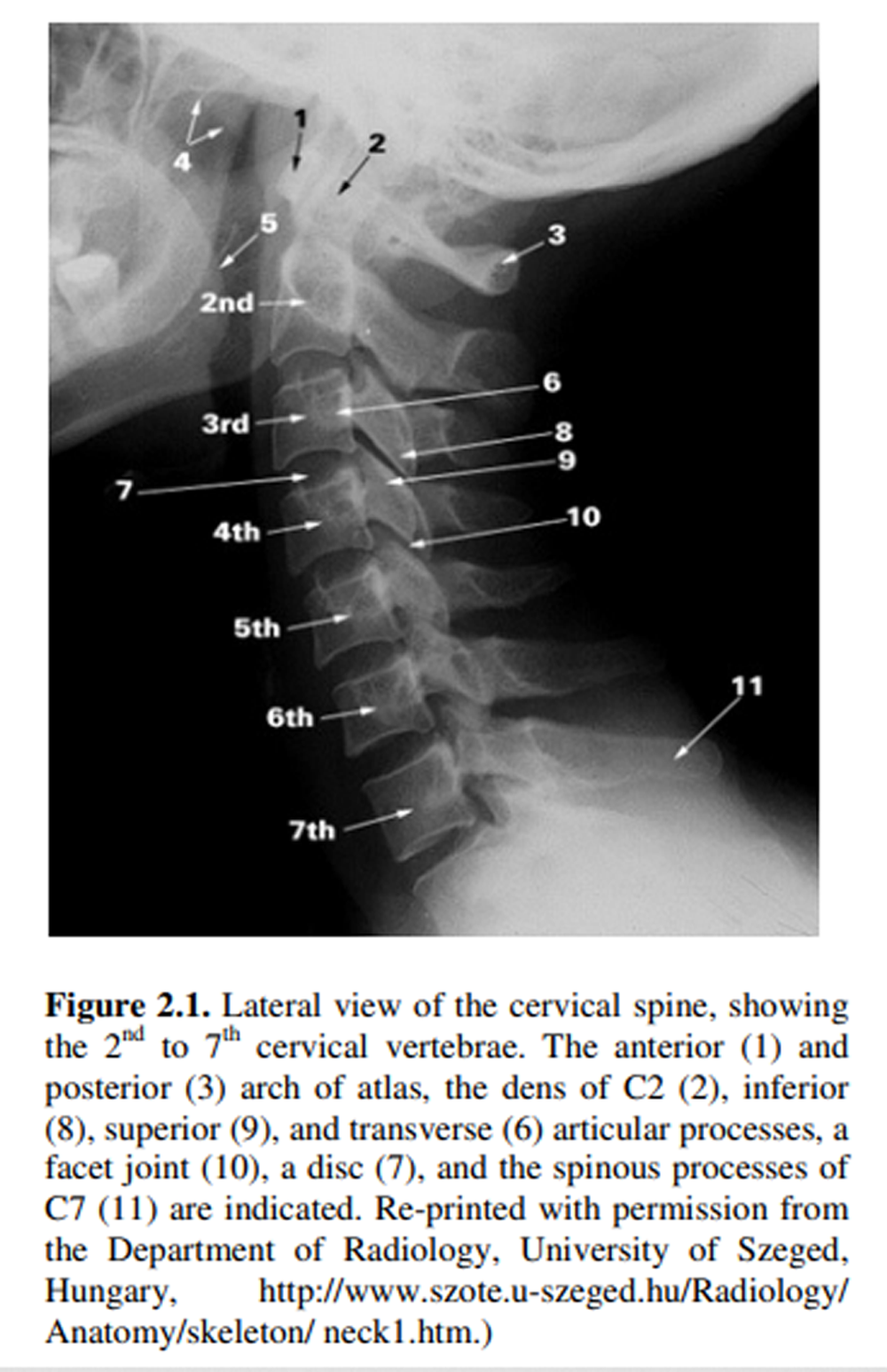
On standard lateral and A-P views, the anterior and posterior soft tissues deserve careful inspection. Signs of widened retrotracheal space, widened retropharyngeal space, displacement of the prevertebral fat stripe, laryngeal dislocation, or tracheal displacement should be sought. Abnormal vertebral alignment may be shown by a loss of the normal lordotic curve or even an acute kyphotic hyperangulation, vertebral body displacement, abnormal dens position, widened interspinous space, or rotation of the vertebral bodies. Abnormal joints may portray unusual IVD-space symmetry or widening of an apophyseal joint space. It is easy to miss lower cervical fractures because they are often obscured on lateral views by the subject’s shoulders if proper precautions are not taken.
INJURY OF THE CERVICAL NERVE ROOTS
Neural dysfunction associated with either acute or chronic subluxation syndromes basically manifest as abnormalities in sensory interpretations and/or motor activities. These disturbances may be through one of two primary mechanisms: direct nerve or nerve root disorders or of a reflex nature.
Contributing and Complicating Factors
The common subluxation picture is rarely pure. It is often superimposed on subclinical processes in the mature patient such as weak or scarred tissue, vertebral instability, osteochondrophytic ridges at the uncovertebral joints, apophyseal thickening and exostosis. Canal encroachment can occur by a buckling ligamentum flavum, spinal stenosis, posterior vertebral body spurs, disc protrusions, dura and dentate thickening, arachnoid cysts, dura and arachnoid adhesions, and ossification of the posterior longitudinal ligament. Loss of disc space, especially in the lower cervical area, may contribute as a source of chronic irritation to an already inflamed root by altering the angulation of the IVF tunnel. The sequence of inflammation, granulation, fibrosis, adhesion formation, and nerve root stricture may follow, along with a loss in root mobility and elasticity. Fortunately for the young, these degenerative changes are not as pronounced during youth.
Motor Aberrations
Nerve root insults from subluxations may manifest as disturbances in motor reflexes and/or muscular strength. Examples include the deep tendon reflexes such as seen in the reduced biceps reflex when involvement occurs between C5 and C6; or the reduced triceps reflex when involvement occurs between C6 and C7. These reflexes must be compared bilaterally to judge whether hyporeflexia is unilateral. Unilateral hyperreflexia is pathognomonic of an upper motor neuron lesion. Prolonged and/or severe nerve root irritation may also produce trophic changes in the tissues supplied.
Interpreting Sensory Irregularities
When direct nerve root involvement occurs on the posterior root of a specific neuromere, it manifests as an increase or a decrease in sensitivity over the dermatome. A typical example is foraminal occlusion or irritating factors exhibited clinically as hyperesthesia, particularly on the dorsal and lateral aspects of the thumb and radial side of the hand, when involvement occurs between C5 and C6. Another example is on the dorsum of the hand, the index and middle fingers, and the ventroradial side of the forearm, thumb, index and middle fingers, when involvement occurs between C6 and C7. In other instances, nerve root involvement may cause hypertonicity and the sensation of deep pain in the muscles supplied by the neuromere. For example, in C6 involvement, there is deep pain in the biceps. In C7 lesions, there is deep pain in the triceps and supinators of the forearm. Direct pressure near the nerve root or along its distribution may be particularly painful.
| Review the complete Chapter (including sketches and Tables) at the ACAPress website |



Hello I am Julia i am 28 years old, and i have reversal of the cervical spine ( i believe). I found this out about a year an a half ago, I was having severe neck pain, and I felt like i was having anxiety. The Pain was so severe i could not even sleep I would be up for days without and when i would sleep i would sleep sitting up with a pillow underneath my chin. I think i has effected a little part of my esophagus because before all of this happened, one day I was sitting in bed and it felt as if I had something tuck in my throat, i panicked and went to the hospital, where they just passed it on as and anxiety attack well this sensation continued for on for several moths until i started having sever pain in my head, at first i noticed i was getting headaches frequently and before that i had maybe 3 headaches a year. now i was having one once a month,Then the pain in my neck started it hurt so bad i could not lay on it at all. I was able to see my nurse practitioner and she had x-rays done. She told me i had reversal of the c-spine, and nothing else about it, she said she was going to refer me to some one and i waited for weeks in chronic pain, I called them and asked if my referral was on the way, she said no it takes a while, so a few weeks later i got it in the mail, and she said there was nothing at this time that that they could do, and i was to go to physical therapy through some one else. I was on a low budget then and could not afford the physical therapy. i then called them and they acted like my neck is not a serious matter. So I just adapted to living with the pain, after a weeks i noticed other things happening, right as i would fall asleep, a sudden jolt of tingling all over my body would wake me up, almost like a entire muscle spasm. After a while it started not to bother me as often and i could sleep better. I still had pain but it wasn’t as severe eventually it got to the point where i just fall asleep on one side and i am fine, no spasm feeling and not a whole lot of pain. I have been good for about 6 months and then in the end of July I was having increasing headaches i would have one about every 5 to 6 days, all i can do is sleep to get rid of them, sometimes medicine will work but usually only sleep. Now the headaches have increased to one a day or one every other day, and the pain in my neck is getting worse day by day, a few days again had another spasm and they scare the heck out of me. I noticed to that i can not hold a pen to long or my arm will go numb, i am in art school this symptom has been going on for about 5 months now, it take about 10 minutes and i lose feeling in my arm. It also seen that hear more crunching sounds in my neck as well. More like crunching and grinding. Last night (jan. 28th 2011) i went to the hospital, because i had such a horrible headache i could not focus at work, so i went there to figure out what was going on with my neck. all they did for me was tell me i had no tumors or anything in my head after they gave me a cat scan then she said you do have a reversed spine but she told me nothing about it and she acted like it was no big deal.
How do i get help for this I am very scared, but i do not know who to see for this, and i am on a low income budget for a few more months until i switch positions at work, I need help, because its getting more painful, the headaches our almost daily and they are bad, and the spasm like things are happening again, i am scared I will become paralyzed, or turn my neck the wrong way some day and snap there i go. I know nothing about this or treatment. I live in the Springfield Illinois area, If i could get some help I would be very thankful_ JULIA
Hi Julia
I had similar problems following a car accident, and in fact that’s what first got me interested in chiropractic.
Our site is not one of those casual “ask-the-doc” pages, and it isn’t realistic to work with someone electronically. I understand how frustrating it is to have a medical person look at your neck and not understand how loss of function is coupled with many of the symptoms you mention.
I believe you would benefit from being assessed by a chiropractor. Meanwhile, you will be in my prayers.
I guess i was asking help for whom i should see :). Its just awful when people or doctors don’t listen or seem to listen. I mean they don;t even driect me who to see, so i guess my biggest thing was to see whom i should see a chiropractor or a orthopedic, Thank you Frank, i will be contacting a Chiropractor.