Medical Physicians Ignore Low Back Pain Guidelines
SOURCE: ChiroACCESS
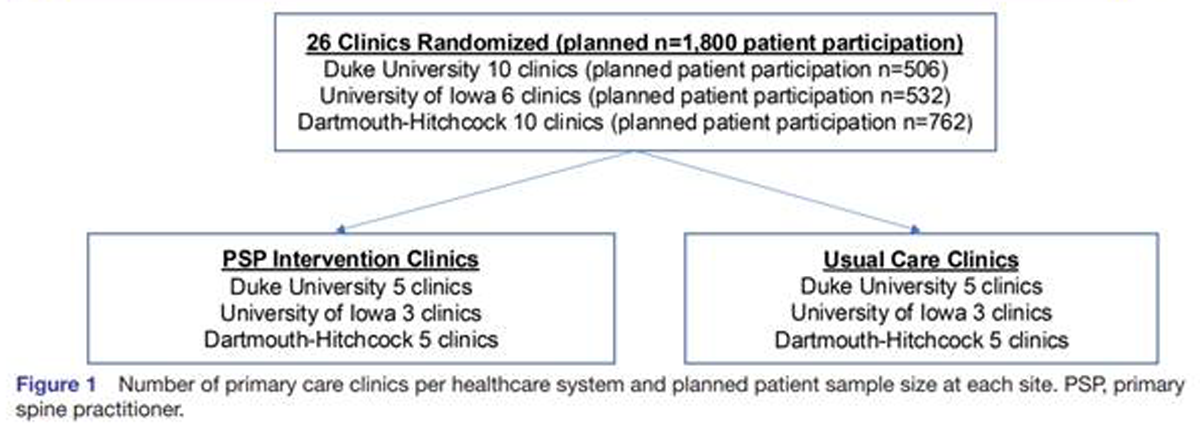
A February 2010 study of 3,533 general practice low back pain patients found that many providers are not following their own evidence based guidelines. [1] Guidelines do provide the overall best evidence but are not meant to be a cookbook approach to care. There is also a need for flexibility so the physician can deviate from guidelines when the specific needs and desires of the patient dictate. In addition, the clinical judgment of the physician may override the guidelines when in a particular patient’s case they are inappropriate.
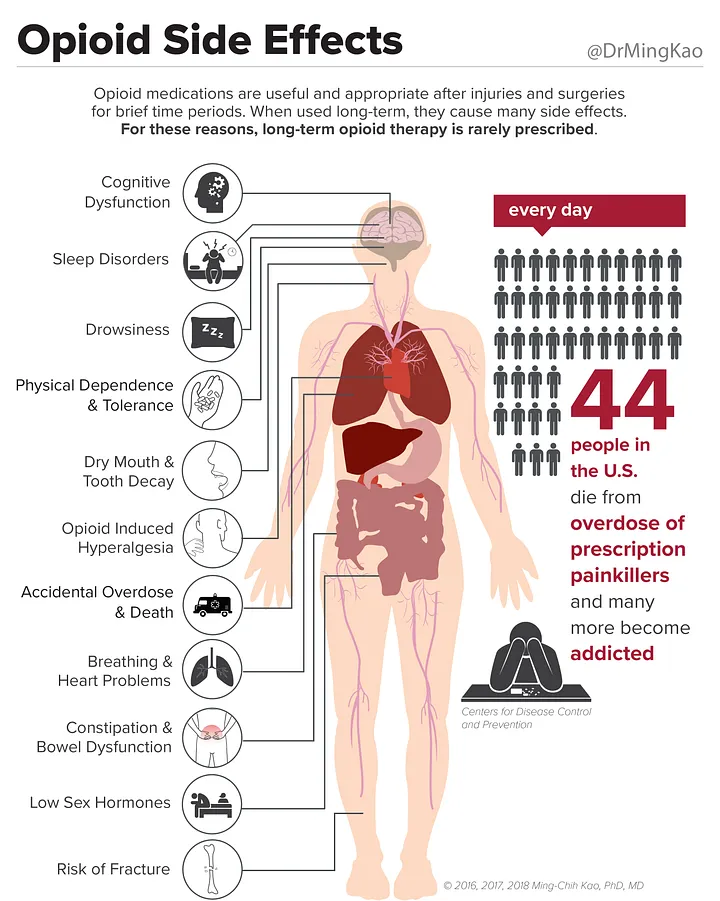
There is, however, reason for concern when risky and or expensive unneeded procedures are used. The medical guideline for acute low back pain call for advice and analgesics, but 80% of the 3,533 patients in this study were not given advise and 82% were not given analgesics. More harmful medications that are not recommended in the guidelines were prescribed, with 37% getting anti-inflammatory drugs and ~20% opiods.
Read the rest of this fascinating review at ChiroACCESS
You may also want to review contemporary research that documents the inadequacy medical training for musculoskeletal conditions.
REFERENCES
1. Low back pain and best practice care: a survey of general practice physicians
Arch Intern Med. 2010 (Feb 8); 170 (3): 271-7




Hi Frank,
You article made me think of this:
http://www.anthonyclose.com/blog/17-when-to-discharge-the-patient
Cheers,
Anthony
A great article, but I doubt this is news to most practicing chiropractors. While PCPs have extensive training they are at times limited in the musculoskeletal field. The question remains as to how we correct this? Research continues to show the effectiveness of exercise therapy, manipulation, and cost effectiveness of conservative care. Yet we see little change in the habits of some health care providers.
I am not taken back by the findings of the presented article yet I am glad to see that this was investigated. I would love to see some numbers on the estimated over-utilzation of imaging by MD’s. A recent review article by Mayer et al. continued to show efficacy for exercise therapy, manipulation, massage, and education for the treatment of back pain as mentioned above. Advising exercise and screening for depression; that should be incorporated into all patient evlauations and treatment plans as per the NCQA guidelines.
Mayer abstract: http://www.ncbi.nlm.nih.gov/pubmed/20071924
Often people are quick to readopt their faulty movement habits and behaviors merely because they are comfortable with them. The faulty movements seem familiar. This is why many practitioners fail with passive treatment. You can do all the manipulation, soft-tissue work, and trigger point therapies you want but the second that person goes home and plops back on to the couch, there goes your work. Re-program the patients faults in movement along side the passive treatments and watch your outcomes improve dramatically.
I couldn’t agree more with Dr. Close. The most difficult part is getting the person to think past the hardware (structural) problem and begin addressing the ‘software problem’ which is most often faulty, repeated movement patterns. Patients who can understand this and become motivated to change their habits respond much faster and with more lasting outcomes.
Active care is a necessary addition to the more passive approaches.