Who Gets Depressed? Who Stays Depressed?
Whiplash-associated Disorders: Who Gets Depressed? Who Stays Depressed?
SOURCE: Eur Spine J. 2010 (Jun); 19 (6): 945–956
Leah A. Phillips, Linda J. Carroll,
J. David Cassidy, and Pierre Côté
Department of Public Health Sciences,
Alberta Centre for Injury Control and Research,
School of Public Health, University of Alberta,
4075 RTF, 8308 114 St, Edmonton, AB, T6G 2E1, Canada.
Depression is common in whiplash-associated disorders (WAD). Our objectives were to identify factors associated with depressive symptomatology occurring in the initial stages of WAD, and to identify factors predicting the course of depressive symptoms. A population-based cohort of adults sustaining traffic-related WAD was followed at 6 weeks, 3, 6, 9, and 12 months. Baseline measures (assessed a median of 11 days post-crash) included demographic and collision-related factors, prior health, and initial post-crash pain and symptoms. Depressive symptomatology was assessed at baseline and at each follow-up using the Centre for Epidemiological Studies Depression Scale (CES-D). We included only those who participated at all follow-ups (n = 3,452; 59% of eligible participants). Using logistic regression, we identified factors associated with initial (post-crash) depression. Using multinomial regression, we identified baseline factors predicting course of depression. Courses of depression were no depression; initial depression that resolves, recurs or persists, and later onset depression. Factors associated with initial depression included greater neck and low back pain severity, greater percentage of body in pain, numbness/tingling in arms/hand, dizziness, vision problems, post-crash anxiety, fracture, prior mental health problems, and poorer general health. Predictors of persistent depression included older age, greater initial neck and low back pain, post-crash dizziness, vision and hearing problems, numbness/tingling in arms/hands, anxiety, prior mental health problems, and poorer general health. Recognition of these underlying risk factors may assist health care providers to predict the course of psychological reactions and to provide effective interventions.
From the FULL TEXT Article:
Introduction
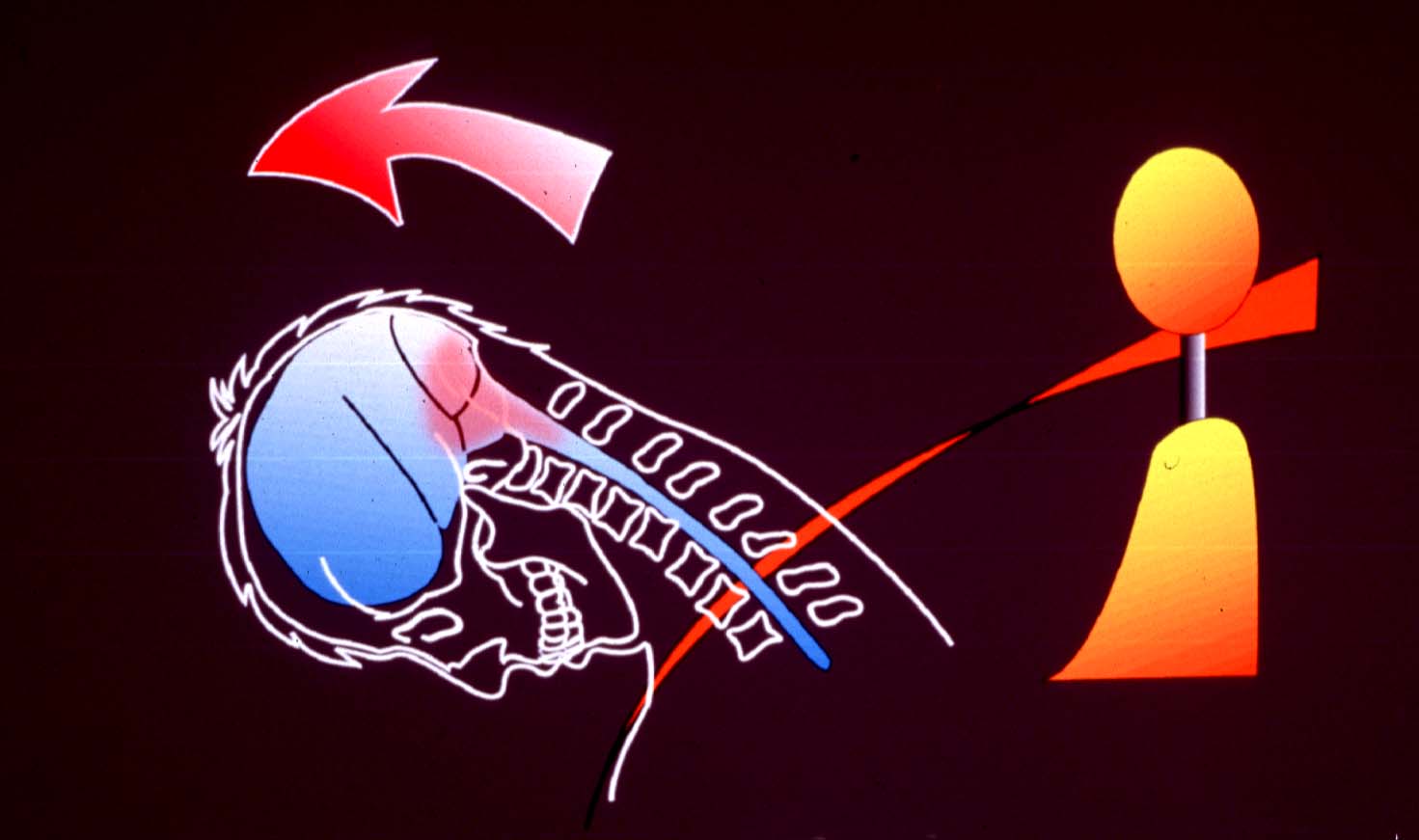
The biopsychosocial model of health posits that in addition to biomedical factors, psychological, and sociological factors play important roles in the diagnosis, treatment, and recovery from illness and disease. [11] According to the Quebec Task Force on whiplash-associated disorders, whiplash is defined as an acceleration–deceleration mechanism of energy transferred to the neck as a result of a motor vehicle collision, and the resulting injury or cluster of symptoms is referred to as whiplash-associated disorders (WAD). [20] WAD is a disorder where the interplay between biological and psychosocial factors appears to have an important effect on recovery. [8]
There are more articles like this @ our: