Conservative Management of Cervicogenic Dizziness Associated With Upper Cervical Instability and Postural Orthostatic Tachycardia Syndrome: A Case Report
SOURCE: Cureus 2024 (Oct 31); 16 (10): e72765
Robert J Trager • Andres Schuster • Cliff Tao • Gina Zamary
Connor Whole Health,
University Hospitals Cleveland Medical Center,
Cleveland, USA.
| OPEN ACCESS |

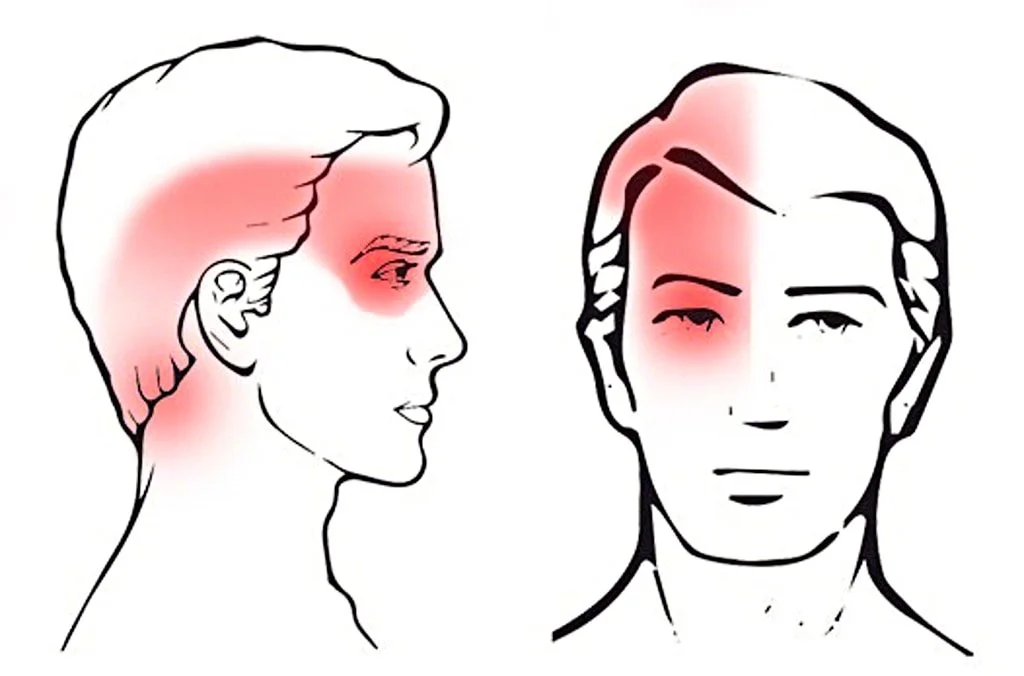
Cervicogenic dizziness (CGD) is a disorder in which dizziness arises from cervical spine dysfunction and is diagnosed after excluding other conditions. We present a case of a 27–year-old woman with a six-year history of dizziness, neck and cervicothoracic pain, and occipital-temporal-orbital headaches. The patient also experienced occasional severe, incapacitating episodes of dizziness with vomiting. Previous evaluations, including advanced imaging, had helped rule out central, otolithic, and psychogenic causes of dizziness. Dynamic radiographs revealed signs of lateral instability of C1 while tilt table testing revealed postural orthostatic tachycardia syndrome (POTS). Over eight months, the patient underwent a regimen of gentle manual therapies and cervical stability exercises. The patient’s dizziness substantially improved, as measured by the Dizziness Handicap Inventory (DHI), with scores reducing from 50 (moderate handicap) to 10 (less than mild handicap). This case highlights the importance of considering cervical spine dysfunction and associated conditions like POTS in the differential diagnosis of chronic dizziness. While conservative management including manual therapy appeared effective in this case for CGD with underlying upper cervical instability and POTS, additional research is needed on this topic.
Keywords: case reports; cervical vertebrae; chiropractic; dizziness; headache; joint instability; neck pain; postural orthostatic tachycardia syndrome; rehabilitation.
From the FULL TEXT Article:
Introduction
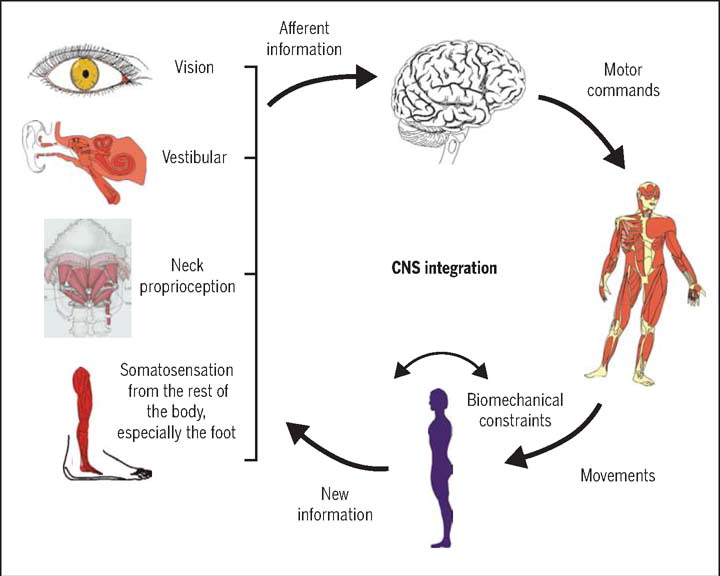
Dizziness is a non-specific term used to describe various sensations, including lightheadedness, unsteadiness, or a spinning feeling. Its utility as a diagnostic term is limited due to its broad nature, necessitating a thorough assessment of the patient’s history and examination for an accurate diagnosis. [1] Dizziness is typically evaluated based on its timing, associated triggers, and symptom subtypes. For instance, benign paroxysmal positional vertigo (BPPV), the most common cause of dizziness, accounting for approximately 24% of cases, presents with brief episodes of rotatory dizziness triggered by head movements. [1, 2] Other subtypes of dizziness may arise from vestibular, vascular, or psychogenic sources, with less frequent causes including Meniere’s disease, vestibular neuritis, and others. [2]
There are more articles like this @
Cervicogenic dizziness (CGD) is defined as a clinical syndrome in which dizziness arises from dysfunction in the cervical spine. [3] Some of the proposed mechanisms of CGD include disc herniations, spondylosis, and upper cervical instability (UCI) at the C1–C2 level. [4–6]
However, diagnosing CGD remains challenging due to the absence of consensus diagnostic criteria and validated tests, making clinical judgment and the exclusion of other causes the primary diagnostic approach. [3, 7] Unlike other forms of dizziness, CGD typically presents with longer-lasting episodes, with symptoms persisting for minutes to hours. [7] Among adults with neck pain, the prevalence of CGD is estimated to be approximately 8.1%. [4]
We present the case of a 27–year-old woman with a six-year history of chronic dizziness, headaches, and neck pain, ultimately diagnosed with CGD associated with C1 lateral instability and underlying postural orthostatic tachycardia syndrome (POTS). This report highlights the importance of recognizing CGD as a differential diagnosis in patients with chronic dizziness and illustrates the clinical improvement following multidisciplinary conservative management.



Leave A Comment