Outcome Measures for Assessing the Effectiveness of Non-pharmacological Interventions in Frequent Episodic or Chronic Migraine: A Delphi Study
SOURCE: BMJ Open. 2020 (Feb 12); 10 (2): e029855
Kerstin Luedtke, Annika Basener, Stephanie Bedei, Rene Castien, Aleksander Chaibi, et al
Pain and Exercise Research,
Universitat zu Lubeck Sektion Medizin,
Lubeck, Germany
kerstin.luedtke@uni-luebeck.de
OBJECTIVES: The aim of this Delphi survey was to establish an international consensus on the most useful outcome measures for research on the effectiveness of non-pharmacological interventions for migraine. This is important, since guidelines for pharmacological trials recommend measuring the frequency of headaches with 50% reduction considered a clinically meaningful effect. It is unclear whether the same recommendations apply to complementary (or adjunct) non-pharmacological approaches, whether the same cut-off levels need to be considered for effectiveness when used as an adjunct or stand-alone intervention, and what is meaningful to patients.
SETTING: University-initiated international survey.
PARTICIPANTS: The expert panel was chosen based on publications on non-pharmacological interventions in migraine populations and from personal contacts. 35 eligible researchers were contacted, 12 agreed to participate and 10 completed all 3 rounds of the survey. To further explore how migraine patients viewed potential outcome measures, four migraine patients were interviewed and presented with the same measurement tools as the researchers.
PROCEDURES: The initial Delphi round was based on a systematic search of the literature for outcome measures used in non-pharmacological interventions for headache.
There are more articles like this @ our:
Suggested outcome measures were rated by each expert, blinded towards the other members of the panel, for its usefulness on a 5–point Likert scale ranging from definitely not useful to extremely useful. Results were combined using median values and IQRs. Tools rated overall as definitely or probably not useful were excluded from subsequent rounds. Experts further suggested additional outcome measures that were presented to the panel in subsequent rounds. Additionally, experts were asked to rank the most useful tools and provide information on feasible cut-off levels for effectiveness for the three highest ranked tools.
RESULTS: Results suggest the use of the Migraine Disability Assessment (MIDAS), Headache Impact Test (HIT-6) and headache frequency as primary outcome measures. Patient experts suggested the inclusion of a measure of quality of life and evaluation of associated symptoms and fear of attacks.
CONCLUSIONS: Recommendations are for the use of the MIDAS, the HIT-6 and headache frequency, in combination with an outcome measure for quality of life. Associated symptoms and fear of attacks should also be considered as secondary outcomes, if relevant for the individual target population. The cut-off level for effectiveness should be lower for non-pharmacological interventions, especially when used as an adjunct to medication.
KEYWORDS: consensus; evaluation; headache; migraine; research
From the FULL TEXT Article:
Introduction
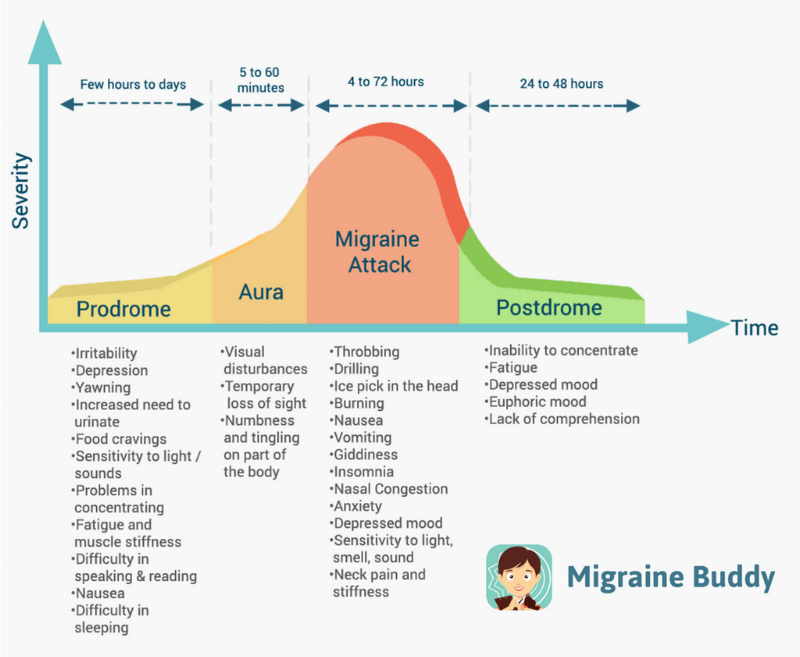
Migraine is a prevalent [1, 2] and disabling condition, [3] with high socioeconomic costs mainly due to days off work. [4–9] Migraine may become chronic when it occurs on ≥15 days per month for at least 3 months with features of migraine in ≥8 days. [10]
Guidelines for chronic and frequent episodic migraine recommend the use of non-pharmacological approaches as an adjunct or alternative to the first-line pharmacological management. [11–16] Patients welcome this recommendation and usually report the use of complementary interventions to reduce the amount of acute pain medication. [17, 18] Especially, those patients who do not tolerate acute and/or prophylactic medicine because of side effects, have contraindications due to co-morbidities or may wish to avoid medication for other reasons, seek non-pharmacological alternatives. [19, 20] Recommended strategies include relaxation, cognitive-behavioural interventions and aerobic exercise; other interventions are mentioned but not recommended due to a lack of evidence for their effectiveness, [11–16] primarily due to methodological shortcomings. [21, 22]
Additional research is urgently needed to identify whether these other non-pharmacological treatment strategies are effective to complement pharmacological management as an adjunct or, in cases where patients do not tolerate acute and/or prophylactic medications because of side effects, have contraindications due to co-morbidities of other diseases or wish to avoid medication for other reasons, can manage their frequent episodic or chronic migraines prophylactically. However, before determining the effectiveness of either intervention, it is important to decide which outcome measures may be useful to indicate change following a non-pharmacological intervention in migraine patients. The International Headache Society (IHS) recommends the use of headache frequency as the primary outcome measure, usually assessed as headache days per month documented in a headache diary. [23]
However, this recommendation refers to studies investigating the effect of preventive medication. A guideline for behavioural trials confirms frequency as the primary outcome measure. [24] No other clinical guidelines determining the main outcome for primary headache disorders exist for non-pharmacological trials. Additionally, no study has investigated whether the number of headache days is an improvement which is meaningful to patients. Therefore, it is unclear whether clinical trials investigating the effectiveness of treatments such as massage, passive mobilisation or manipulation, physical activity or any other non-pharmacological intervention as an adjunct or as a stand-alone intervention should also use headache frequency as a primary outcome measure, and at what cut-off level the intervention can be considered successful.
The cut-off level stated by the IHS and the guideline for behavioural treatment for the effectiveness of a treatment is a reduction of ≥50% of headache frequency. [23, 24] Both guidelines, however, acknowledge that these levels might be lowered for studies on chronic migraine populations or reported as ‘somewhat improved’ if a responder rate >25% is reached. Non-pharmacological interventions have a low risk of adverse events (AEs) and are less expensive. Intuitively, these approaches should therefore not be measured on the same scale as preventive medication since medication has a high risk of AEs. To reach a 50% level of improvement is particularly unrealistic if non-pharmacological interventions are evaluated as an add-on to the pharmacological management, especially since the net effect would then need to reach 75%.
The objective for this Delphi survey was to establish an international consensus on the most useful outcome measures for assessing the effectiveness of non-pharmacological interventions for frequent episodic or chronic migraine. A secondary aim of the Delphi study was to investigate whether the same level of improvement, that is, ≥50% in headache frequency, is required to conclude on its effectiveness as recommended for preventative migraine medication, when used as an adjunct or a stand-alone intervention.
Read the rest of this Full Text article now!



Leave A Comment