Nonpharmacological Treatment of Army Service Members with Chronic Pain Is Associated with Fewer Adverse Outcomes After Transition to the Veterans Health Administration
SOURCE: J Gen Intern Med. 2019 (Oct 28) [Epub]
Esther L. Meerwijk, PhD, MSN , Mary Jo Larson, PhD, MPA, Eric M. Schmidt, PhD, Rachel Sayko Adams, PhD, MPH, Mark R. Bauer, MD, Grant A. Ritter, PhD, Chester Buckenmaier III, MD, and Alex H. S. Harris, PhD, MS
VA Health Services Research & Development,
Center for Innovation to Implementation (Ci2i),
VA Palo Alto Health Care System,
Menlo Park, CA, USA.
BACKGROUND: Potential protective effects of nonpharmacological treatments (NPT) against long-term pain-related adverse outcomes have not been examined.
OBJECTIVE: To compare active duty U.S. Army service members with chronic pain who did/did not receive NPT in the Military Health System (MHS) and describe the association between receiving NPT and adverse outcomes after transitioning to the Veterans Health Administration (VHA).
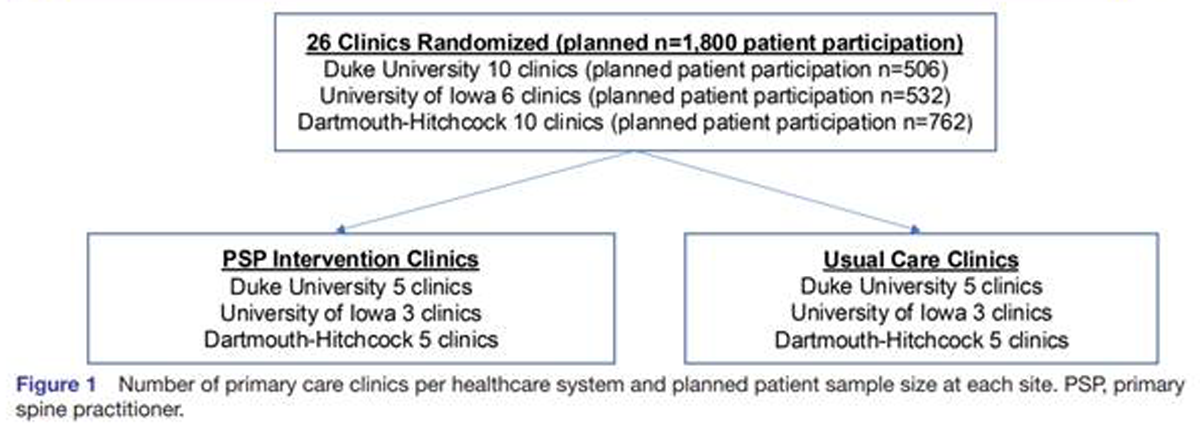
DESIGN AND PARTICIPANTS: A longitudinal cohort study of active duty Army service members whose MHS healthcare records indicated presence of chronic pain after an index deployment to Iraq or Afghanistan in the years 2008-2014 (N = 142,539). Propensity score-weighted multivariable Cox proportional hazard models tested for differences in adverse outcomes between the NPT group and No-NPT group.
EXPOSURES: NPT received in the MHS included acupuncture/dry needling, biofeedback, chiropractic care, massage, exercise therapy, cold laser therapy, osteopathic spinal manipulation, transcutaneous electrical nerve stimulation and other electrical manipulation, ultrasonography, superficial heat treatment, traction, and lumbar supports.
There are more articles like this @ our:
MAIN MEASURES: Primary outcomes were propensity score-weighted proportional hazards for the following adverse outcomes: (a) diagnoses of alcohol and/or drug disorders; (b) poisoning with opioids, related narcotics, barbiturates, or sedatives; (c) suicide ideation; and (d) self-inflicted injuries including suicide attempts. Outcomes were determined based on ICD-9 and ICD-10 diagnoses recorded in VHA healthcare records from the start of utilization until fiscal year 2018.
KEY RESULTS: The propensity score-weighted proportional hazards for the NPT group compared to the No-NPT group were 0.92 (95% CI 0.90-0.94, P < 0.001) for alcohol and/or drug use disorders; 0.65 (95% CI 0.51-0.83, P < 0.001) for accidental poisoning with opioids, related narcotics, barbiturates, or sedatives; 0.88 (95% CI 0.84-0.91, P < 0.001) for suicide ideation; and 0.83 (95% CI 0.77-0.90, P < 0.001) for self-inflicted injuries including suicide attempts.
CONCLUSIONS: Nonpharmacological treatments (NPT) provided in the Military Health System (MHS) to service members with chronic pain may reduce risk of long-term adverse outcomes.
KEYWORDS: adverse outcomes; chronic pain; nonpharmacological treatment; opioids; veterans
From the FULL TEXT Article:
INTRODUCTION
Chronic pain is a costly public health issue that is associated with many adverse outcomes including chronic opioid use and suicide. [1] Deployment to conflict zones places military service members at risk for chronic pain, which often persists after they leave military service and transition their healthcare from the Military Health System (MHS) to the Veterans Health Administration (VHA). [2, 3] Twenty-nine percent to 44% of active duty service members reported chronic pain after deployment to conflict zones in Iraq or Afghanistan, and 48 to 60% of VHA primary care patients reported chronic pain. [4–7] Chronic pain is a well-established risk factor for suicide ideation and suicide attempts, as well as for opioid use disorder and opioid-related overdose, especially in the presence of already existing substance use disorder. [8, 9]
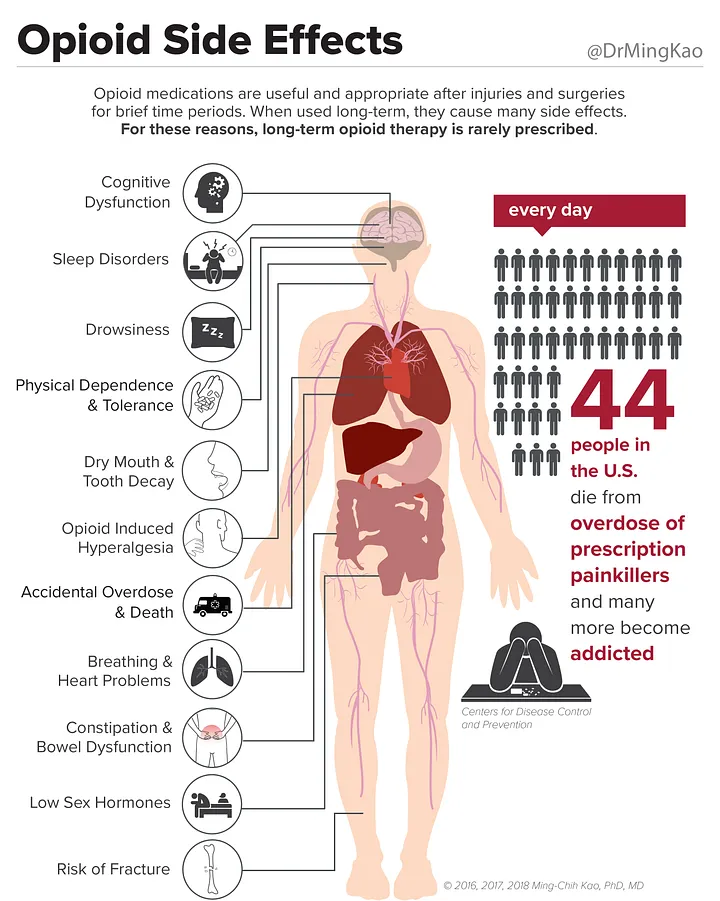
Chronic pain is often managed with prescription opioids which, especially at higher doses and/or longer duration of use, have been associated with increased risk for substance use disorders, opioid-related overdose, self-inflicted injuries, and suicide attempts. [10–16] In addition to opioids, chronic pain can be managed with nonpharmacological treatments (NPT). [17–19] These include treatments like exercise therapy and chiropractic manipulation, as well as less common treatments, like yoga, massage, and acupuncture. [20] Compelling evidence for a moderate effect on clinical outcomes was found for exercise and spinal manipulation in nonmilitary samples with chronic low back pain, although the effect on pain intensity was small to moderate and mostly short-term. [21, 22] Recent research in active duty service members showed that early NPT was associated with a lower risk of military duty limitations, and facilities where NPT was more common were less likely to initiate long-term opioid treatment for their patients. [23, 34]
If NPT is used to manage chronic pain, in addition to or instead of opioids, thismay not only have an effect on pain and functional status, but also on adverse outcomes that are associated with chronic pain and opioid use, such as substance use disorders, drug overdose, and self-inflicted injuries. The potential long-term protective effect of NPT against adverse outcomes has not been examined. The purpose of the current analyses was to compare active duty U.S. Army service members with chronic pain who did and did not receive NPT in the MHS and describe the association between receiving NPT in theMHS and adverse outcomes observed after transition to the VHA, specifically alcohol and drug abuse or dependence, accidental or intentional drug poisoning, suicide ideation, and self-inflicted injuries.
Studying these outcomes broadens our knowledge of the potential impacts of NPT beyond their effect on pain and provides valuable information to support clinical decision-making regarding chronic pain management. Studying outcomes after transition to VHA allows for longterm observation and highlights the potential cross-system impacts of NPT. We hypothesized that the use of NPT in the MHS would be associated with a lower likelihood of adverse outcomes in the VHA. These analyses are part of the Substance Use and Psychological Injury Combat Study (SUPIC), the largest longitudinal, observational study to date of pain management and behavioral health conditions using MHS data from U.S. Army service members returning from deployments in support of Operations Enduring Freedom (OEF), Iraqi Freedom (OIF), and New Dawn (OND). [25]
Read the rest of this Full Text article now!





Leave A Comment