Chiropractic Treatment Including Instrument-assisted Manipulation for Non-specific Dizziness and Neck Pain in Community-dwelling Older People: A Feasibility Randomised Sham-controlled Trial
SOURCE: Chiropractic & Manual Therapies 2018 (May 10); 26: 14
Julie C. Kendall, Simon D. French, Jan Hartvigsen, and Michael F. Azari
School of Health and Biomedical Sciences,
RMIT University,
PO Box 71 Bundoora,
Melbourne, VIC 3083 Australia.
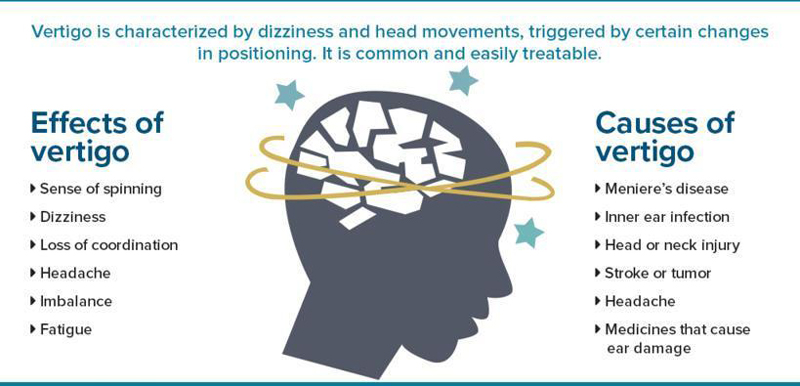
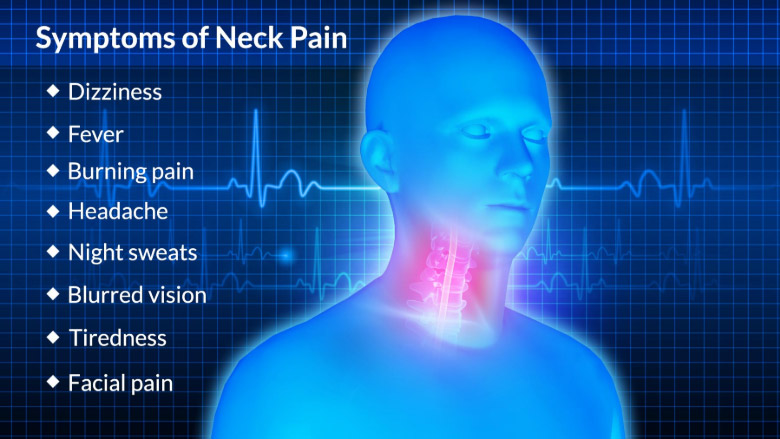
BACKGROUND: Dizziness in older people is a risk factor for falls. Neck pain is associated with dizziness and responds favourably to neck manipulation. However, it is unknown if chiropractic intervention including instrument-assisted manipulation of the neck in older people with neck pain can also improve dizziness.
METHODS: This parallel two-arm pilot trial was conducted in Melbourne, Australia over nine months (October 2015 to June 2016). Participants aged 65–85 years, with self-reported chronic neck pain and dizziness, were recruited from the general public through advertisements in local community newspapers and via Facebook. Participants were randomised using a permuted block method to one of two groups: 1) Activator II™-instrument-assisted cervical and thoracic spine manipulation plus a combination of: light massage; mobilisation; range of motion exercises; and home advice about the application of heat, or 2) Sham-Activator II™-instrument-assisted manipulation (set to zero impulse) plus gentle touch of cervical and thoracic spinal regions. Participants were blinded to group allocation. The interventions were delivered weekly for four weeks. Assessments were conducted one week pre- and post-intervention. Clinical outcomes were assessed blindly and included: dizziness (dizziness handicap inventory [DHI]); neck pain (neck disability index [NDI]); self-reported concerns of falling; mood; physical function; and treatment satisfaction. Feasibility outcomes included recruitment rates, compliance with intervention and outcome assessment, study location, success of blinding, costs and harms.
RESULTS: Out of 162 enquiries, 24 participants were screened as eligible and randomised to either the chiropractic (n = 13) or sham (n = 11) intervention group. Compliance was satisfactory with only two participants lost to follow up; thus, post-intervention data for 12 chiropractic intervention and 10 sham intervention participants were analysed. Blinding was similar between groups. Mild harms of increased spinal pain or headaches were reported by 6 participants. Costs amounted to AUD$2635 per participant. The data showed a trend favouring the chiropractic group in terms of clinically-significant improvements in both NDI and DHI scores. Sample sizes of n = 150 or n = 222 for dizziness or neck pain disability as the primary outcome measure, respectively, would be needed for a fully powered trial.
There are more articles like this @ our:
CONCLUSIONS: Recruitment of participants in this setting was difficult and expensive. However, a larger trial may be feasible at a specialised dizziness clinic within a rehabilitation setting. Compliance was acceptable and the outcome measures used were well accepted and responsive.
TRIAL REGISTRATION: Australian New Zealand Clinical Trials Registry (ANZCTR) ACTRN12613000653763.
Registered 13 June 2013.
Trial funding: Foundation for Chiropractic Research and Postgraduate Education (Denmark).
KEYWORDS: Chiropractic; Dizziness; Elderly; Neck pain; Randomised controlled trial
From the FULL TEXT Article:
Background
Dizziness and musculoskeletal pain are common in older people [1–4] and are associated with postural instability [5], fear of falling [6–8], and increased incidence of falls. [9–12] Among Australian adults, 36% of people aged over 50 years report the presence of dizziness within the last month. [13] Similarly, the prevalence of neck pain in Australian older adults has been estimated at 36% and 41% for men and women respectively [14], and in older adults, 5% of men and 8% of women report that neck pain interferes with their physical activity. [2]
Dizziness is a known risk factor for falls in community-dwelling older people [11], and dizziness is not optimally managed at present. One in three older people with dizziness are prescribed medications that are known to increase the risk of falling including: anti-hypertensives; anxiolytics and antidepressants; nitrates; analgesics; and anti-vertigo medications. [15] Anti-vertigo medications in particular, are commonly prescribed for non-vestibular causes of dizziness. [16] Therefore, there is a need to develop and validate non-pharmacological treatment strategies for dizziness in this population, which in turn may reduce the need for prescription of pharmacological agents with their attendant potential side-effects. [15, 17]
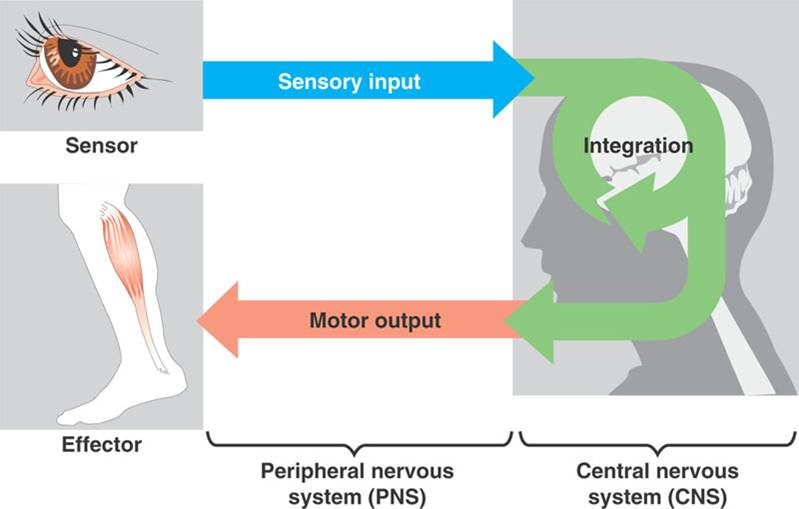
Neck pain may increase the risk of falls in the elderly. Sensory information from various structures including the vestibular apparatus in the inner ear, the eyes, and the proprioceptive receptors in muscles and joints, particularly of the neck, is integrated by the brain for position sense, balance and motor control. [18] In some individuals, neck pain is linked with dizziness, in a syndrome termed ‘cervicogenic dizziness’ or ‘cervical dizziness’. [19–21] There are reports in neck pain patients of a correlation between cervical joint stiffness and hypertonicity of the upper cervical musculature and the presence of dizziness. [22–24] There are many different causes of dizziness in older people, including vestibular, cardiovascular, and psychological. [25] In addition, since cervicogenic dizziness is a diagnosis of exclusion, its exact incidence and prevalence remain unknown and a definitive diagnosis of cervicogenic dizziness is not possible in primary care settings. Therefore, this study recruited older people who reported both chronic non-specific dizziness and chronic neck pain to optimise the relevance of the study findings for primary care settings.
Read the rest of this Full Text article now!


Leave A Comment