The Biopsychosocial Model and Chiropractic:
A Commentary with Recommendations for
the Chiropractic Profession
SOURCE: Chiropractic & Manual Therapies 2017 (Jun 7); 25: 16
Jordan A. Gliedt, Michael J. Schneider, Marion W. Evans, Jeff King and James E. Eubanks Jr
College of Chiropractic,
Logan University
There is an increasing awareness, interest and acceptance of the biopsychosocial (BPS) model by all health care professionals involved with patient care. The areas of spine care and pain medicine are no exception, and in fact, these areas of health care are a major centerpiece of the movement from the traditional biomedical model to a BPS model of patient assessment and delivery of care. The chiropractic approach to health care has a history that is grounded in key aspects of the BPS model. The profession has inherently implemented certain features of the BPS model throughout its history, perhaps without a full understanding or realization. The purpose of this paper is to present an overview of the BPS model, its relationship with spine care and pain management, and to discuss the BPS model, particularly psychosocial aspects, in the context of its historical relationship with chiropractic. We will also provide recommendations for the chiropractic profession as it relates to successful adoption of a full integration of the BPS model.
There are more articles like this @ our:
KEYWORDS: Biopsychosocial Biomedical Chiropractic Back pain Neck pain Pain management
From the FULL TEXT Article
Background
Biological influences are an important component of health and disease, particularly in the area of spine care and pain management. Acknowledging this aspect of patient presentation holds value in guiding appropriate management approaches. Appreciation of the psychological and social aspects of patient care carries significance as well and should not be overlooked. The objective of this paper is to provide an overview of the biopsychosocial (BPS) model and predominantly the psychosocial components of spine care, pain management, and the chiropractic profession. The authors recognize the importance of the biological element of health and disease, particularly in the fields of spine and pain care. The central focus of this paper, however, is on the psychological and to a lesser extent social aspects because, as illustrated in this paper, these are not fully appreciated in chiropractic at this time.
The biopsychosocial model
The notion of psychological and social determinants contributing to the development, persistence and healing of illness is not novel. Discussions of psychosocial influences in health and disease have been noted for multiple centuries. [1, 2] A noteworthy example is Francis Peabody’s famous speech, “The Care of the Patient”, given to attendees of Harvard Medical School in 1927 which specifically addressed the importance of the art of patient-centered medicine that extends beyond the impersonal scientific mechanisms of the treatment of disease. [3] Interestingly, this dialogue is reflective of chiropractic philosophy which has regularly emphasized the art and science of chiropractic care which includes a whole person approach that aims to investigate, eliminate, and prevent the cause of disease.
Despite historical considerations of the potential for psychosocial impact on physical well-being, the majority of the twentieth century was governed by the biomedical model. This model, also known as the pathoanatomic model, resulted from Virchow’s deduction that all disease results from cellular aberration. [4] This mechanistic paradigm played a crucial role in the successful eradication of numerous infectious diseases, with the result of significant extension in life expectancy seen in the twentieth century. Since many biomedically-responsive problems have now been addressed successfully, health care as a whole has begun to turn its attention to quality of life issues that require a new model of care.
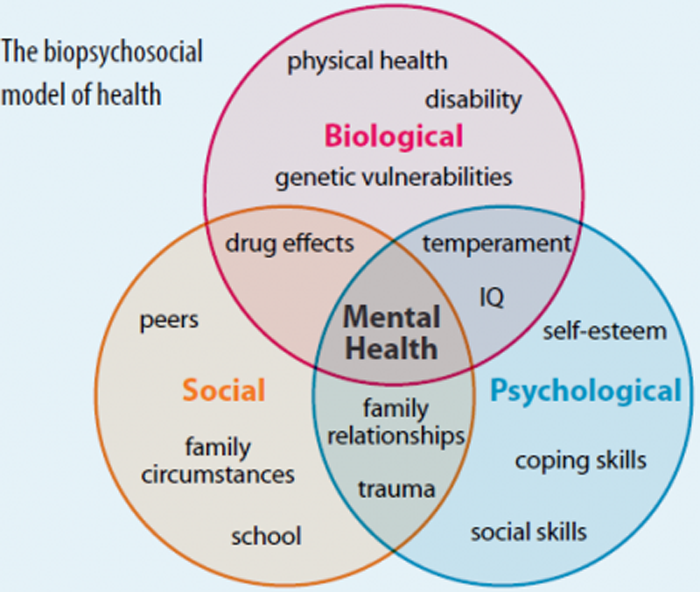
The last few decades have seen considerable attention and acceptance of psychosocial influences in health, exemplified by the BPS model. [5] The development of the BPS model is attributed to Engel’s challenge of the biomedical model in 1977. [6] Engel argued that the biomedical model leaves no room for appreciation of psychosocial considerations in disease and therefore “distorts perspectives and even interferes with patient care”. [6] Engel proposed a new medical model that intertwined biological, psychological, and sociological factors: physical or chemical alterations to the body (biological factors), personal development and psychological/mental health factors, and social determinants [6] (Fig. 1).
Read the rest of this Full Text article now!




Leave A Comment