Deconstructing Chronic Low Back Pain in the Older Adult – Step by Step Evidence and Expert-Based Recommendations for Evaluation and Treatment.
Part IV: Depression
SOURCE: Pain Medicine 2015 (Nov); 16 (11): 2098-2108 ~ FULL TEXT
Joseph A. Carley, Jordan F. Karp, Angela Gentili,
Zachary A. Marcum, M. Carrington Reid, Eric Rodriguez,
Michelle I. Rossi, Joseph Shega, Stephen Thielke,
Debra K. Weiner
Departments of Psychiatry,
University of Pittsburgh,
Pittsburgh, PA, USA
This is just one from a series of 10 articles titled:
OBJECTIVE: To present the fourth in a series of articles designed to deconstruct chronic low back pain (CLBP) in older adults. The series presents CLBP as a syndrome, a final common pathway for the expression of multiple contributors rather than a disease localized exclusively to the lumbosacral spine. Each article addresses one of twelve important contributors to pain and disability in older adults with CLBP. This article focuses on depression.
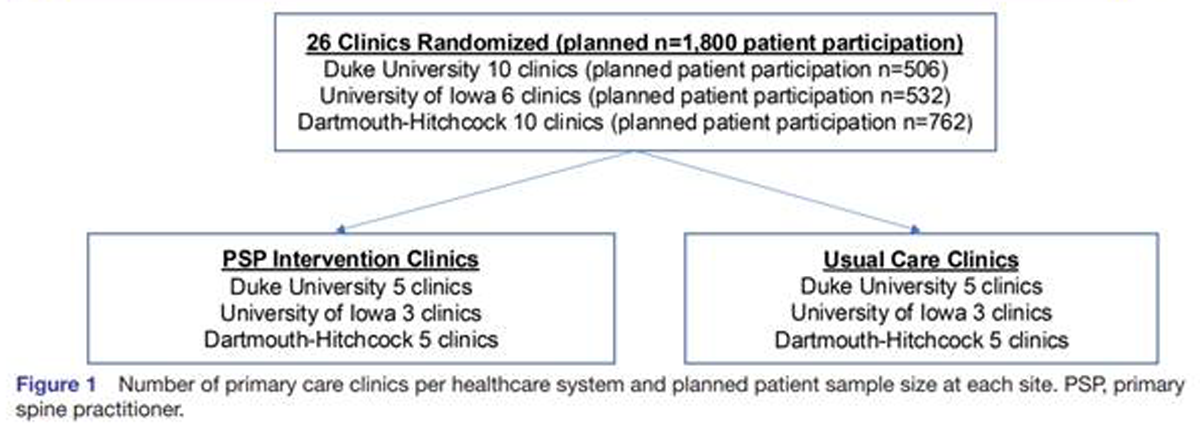
METHODS: The evaluation and treatment algorithm, a table articulating the rationale for the individual algorithm components, and stepped-care drug recommendations were developed using a modified Delphi approach. The Principal Investigator, a three-member content expert panel, and a nine-member primary care panel were involved in the iterative development of these materials. The algorithm was developed keeping in mind medications and other resources available within Veterans Health Administration (VHA) facilities. As panelists were not exclusive to the VHA, the materials can be applied in both VHA and civilian settings. The illustrative clinical case was taken from one of the contributor’s clinical practice.
RESULTS: We present an algorithm and supportive materials to help guide the care of older adults with depression, an important contributor to CLBP. The case illustrates an example of a complex clinical presentation in which depression was an important contributor to symptoms and disability in an older adult with CLBP.
There are more articles like this @ our:
CONCLUSIONS: Depression is common and should be evaluated routinely in the older adult with CLBP so that appropriately targeted treatments can be planned and implemented.
KEYWORDS: Aged; Assessment; Chronic Pain; Depression; Elderly; Low Back Pain; Primary Care
From the FULL TEXT Article:
Introduction
Major depressive disorder (MDD) has a reported 1-year prevalence of 6–12% in older adults in both Veterans Affairs and civilian settings. In addition to MDD, the prevalence of clinically significant subsyndromal depressive symptoms in late-life (generally defined as ≥65 years) is estimated to be even higher. This may be due to under-recognition in the context of complex comorbidities. [1, 2] Depression is often a recurrent illness, triggered, and exacerbated by both psychological stress and medical illnesses. High medical burden in older adults contributes to treatment response variability such as delayed response to antidepressant pharmacotherapy and increased likelihood of recurrence. [3]
Numerous studies suggest that depression worsens both the severity of and disability caused by chronic low back pain (CLBP). [4-8] A large survey of community dwelling older adults found that mild to severe depressive symptoms increased the odds of disabling low back pain over a period of 2 years by 30–60%. [8] Similarly, baseline disabling low back pain ranging from a little of the time to all of the time increased the odds of depressive symptoms by 27.9–84.2%, respectively. [8] As depression is a treatable illness, a rational approach to reducing the burden of CLBP is to diagnose and treat comorbid depression. To date, there is little research published about how to assess and treat these conditions simultaneously.
Read the rest of this Full Text article now!




Leave A Comment