Deconstructing Chronic Low Back Pain in the Older Adult – Step by Step Evidence and Expert-Based Recommendations for Evaluation and Treatment.
Part II: Myofascial Pain
SOURCE: Pain Medicine 2015 (Jul); 16 (7): 1282-1289 ~ FULL TEXT
Anthony J. Lisi, Paula Breuer, Rollin M. Gallagher,
Eric Rodriguez, Michelle I. Rossi, Kenneth Schmader,
Joel D. Scholten, Debra K. Weiner
VA Connecticut Healthcare System
2Rehabilitation and Prosthetics Services,
Veterans Health Administration.
3University of Bridgeport College of Chiropractic
This is just one from a series of 10 articles titled:
OBJECTIVE: To present an algorithm of sequential treatment options for managing myofascial pain (MP) in older adults, along with a representative clinical case.
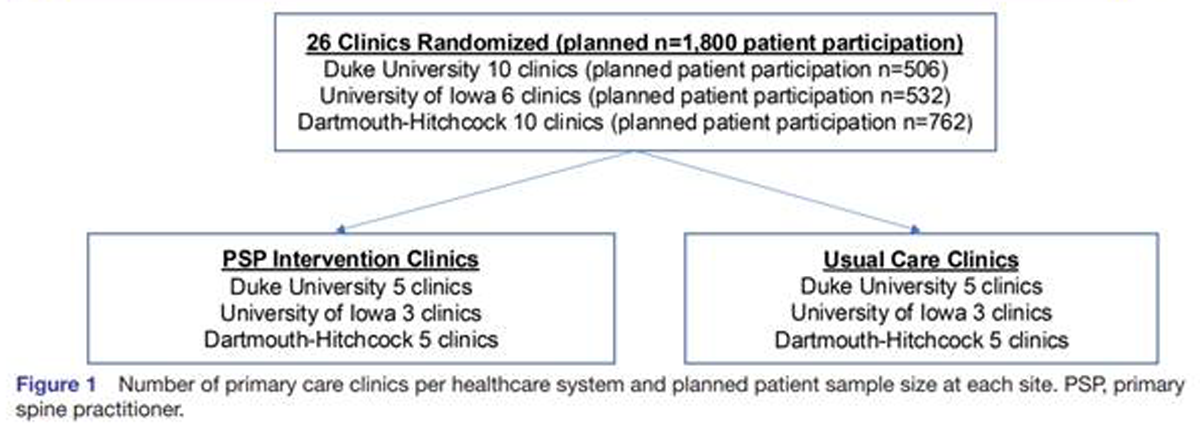
METHODS: A modified Delphi process was used to synthesize evidence-based recommendations. A multidisciplinary expert panel developed the algorithm, which was subsequently refined through an iterative process of input from a primary care physician panel.
RESULTS: We present an algorithm and supportive materials to help guide the care of older adults with MP, an important contributor to chronic low back pain (CLBP). Addressing any perpetuating factors should be the first step of managing myofascial pain (MP). Patients should be educated on self-care approaches, home exercise, and the use of safe analgesics when indicated. Trigger point deactivation can be accomplished by manual therapy, injection therapy, dry needling, and/or acupuncture.
There are more articles like this @ our:
CONCLUSIONS: The algorithm presented gives a structured approach to guide primary care providers in planning treatment for patients with MP as a contributor to CLBP.
KEYWORDS: Chronic Low Back Pain; Chronic Pain; Degenerative Disc Disease; Elderly; Low Back Pain; Lumbar; Myofascial Pain; Older Adults; Pain Disorder; Spinal Stenosis
From the FULL TEXT Article:
Introduction
Myofascial pain (MP) as first described by Travell and Simons, is defined by a localized region of palpable tightness and tenderness within a muscle that is characterized by resistance to passive elongation, and reproduction of a predictable pattern of referred pain on palpation. [1] The pathogenesis of MP is not fully understood, but can be a local muscle response to underlying mechanical factors (postural abnormalities, biomechanical faults, chronic strain), or a response to altered neurotrophic factors secondary to spondylosis. [2-4]
A characteristic feature of MP is the presence of localized palpable tender regions called trigger points (TrP). These have been identified on microscopic evaluation of involved muscles [5] and exhibit a distinct biochemical profile (i.e., inflammatory mediators, neuropeptides, cytokines, and catecholamines) as compared with normal muscles. [6, 7] The elevated tissue tension in TrP was shown to be decreased by the administration of general anesthesia, supporting a spinal segmentally mediated etiology. [8] It has also been proposed that TrP may have a bidirectional relationship with central sensitization, being both a cause as well as an effect. Preliminary evidence suggests the prolonged nociceptive input from TrP can sensitize dorsal horn neurons, whereas the referred pain phenomenon seen in TrP may in fact be the result of central sensitization. [9]
Read the rest of this Full Text article now!




Leave A Comment