Mild Traumatic Brain Injury and Concussion: An Invisible and Confusing Condition
SOURCE: ACA News ~ June 2015 ~ FULL TEXT
By James J. Lehman, DC, FACO
Traumatic brain injuries are perplexing and problematic — and they affect millions of Americans. It has been estimated that up to 3.8 million Americans incur mild traumatic brain injuries (MTBI) or concussions in sports-related activities and approximately 50 percent of the injured do not report the injury to a health care professional. [1] I suspect that millions of MTBI are not reported to health care providers as a result of sporting activities, motor vehicle accidents, work-related injuries and military operations. Another report claims that MTBI affects more than 1.125 million Americans.
Traumatic brain injury is frequently referred to as the silent epidemic because the problems that result from it (e.g., impaired memory) often are not visible. Mild traumatic brain injury (MTBI) accounts for at least 75 percent of all traumatic brain injuries in the United States.
According to existing data, more than 1.5 million people experience a traumatic brain injury (TBI) each year in the United States. These injuries may cause long-term or permanent impairments and disabilities. Many people with MTBI have difficulty returning to routine, daily activities and may be unable to return to work for many weeks or months. In addition to the human toll of these injuries, MTBI costs the nation nearly $17 billion each year. [2]
Some of the current definitions, position statements and evidence-based guidelines regarding concussion and mild traumatic brain injury are offered for your perusal and consideration. Sources discussing treatment, prevention and living with traumatic brain injuries are provided for those interested in more detail, continuing education credits and certification. The goal of this article is to make more visible your patients with obscure MTBI symptoms. I hope that this article will reduce confusion regarding the diagnosis and treatment of patients with MTBI and concussions.
Bloodless Concussion: The Misunderstood Injury
Some 11 years ago, an excellent review, Bloodless Concussion: The Misunderstood Injury, pointed out that approximately two-thirds of all chiropractic physicians practicing in the United States are licensed to diagnose and treat patients as portal-ofentry health care providers. Consequently, they can assume a major role in evaluating, diagnosing and treating concussions, particularly head injuries that affect the spine and related extremities. The review by David Martinez, DC, focused on concussion and MTBI primarily related to sports injury and chiropractic medicine. He mentioned that it is difficult to diagnose concussion and oftentimes perceived as unimportant because no blood or other obvious clinical signs are visible. [3]
Brain Injuries and Consciousness
The Glasgow Coma Scale (GCS) is the most common scoring system used to describe the level of consciousness in a person following a traumatic brain injury. The GCS is a reliable and objective way of recording the initial and subsequent level of consciousness in a person after a brain injury. [4] Most often it is used in the emergency department and intensive care units. To learn more about the practical method for assessing impairment of consciousness level in response to defined stimuli, go to the website www.glasgowcomascale.org for “GCS at 40.” The website offers a new structured schema, which reinforces a standard approach to assessment that enhances the consistency of its use. It provides the most recent literature, a video explanation and a self-test.
MTBI and Concussion
- The American Medical Society for Sports Medicine defines concussion as a traumatically induced transient disturbance of brain function and involves a complex pathophysiological process. Concussion is a subset of mild trau- matic brain injury (MTBI) that is generally selflimited and at the less severe end of the brain injury spectrum.
- The National Center for Injury Prevention and Control recommends the conceptual definition of MTBI as an injury to the head due to a blunt trauma or acceleration/deceleration forces that result in one or more of the following signs or symptoms:Any period of observed or self-reported:
- Transient confusion, disorientation or impaired consciousness;
- Dysfunction of memory around the time of injury;
- Loss of consciousness lasting less than 30 minutes;
- Observed signs of neurological or neuropsychological dysfunction, such as:
a. Seizures acutely following injury to the head;b. Among infants and very young children: irritability, lethargy or vomiting following head injury;c. Symptoms among older children and adults such as headache, dizziness, irritability, fatigue or poor concentration, when identified soon after injury, can be used to support the diagnosis of mild TBI but cannot be used to make the diagnosis in the absence of loss of consciousness or altered consciousness. Research may provide additional guidance in this area.
- The consensus statement on concussion in sport at the 4th International Conference on Concussion in Sport held in Zurich describes concussion as a brain injury and a complex pathophysiological process affecting the brain, induced by biomechanical forces. Several common features that incorporate clinical, pathological and biomechanical injury constructs may be utilized in defining the nature of a concussive head injury:
- Concussion may be caused by a direct blow to the head, face, neck or elsewhere on the body with an “impulsive” force transmitted to the head.
- Concussion typically results in the rapid onset of short-lived impairment of neurologic function that resolves spontaneously. However, in some cases, symptoms and signs may evolve over a number of minutes to hours.
- Concussion may result in neuropathological changes, but the acute clinical symptoms largely reflect a functional disturbance rather than a structural injury, and, as such, no abnormality is seen on standard structural neuroimaging studies.
- Concussion results in a graded set of clinical symptoms that may or may not involve loss of consciousness. Resolution of the clinical and cognitive symptoms typically follows a sequential course. However, it is important to note that in some cases symptoms may be prolonged. [5]
Posture and Gait Changes Post-Concussion
Almost ten years ago, one study demonstrated that the effects of cerebral concussion on postural control persist for longer than three to four days, even among athletes with no signs of unsteadiness. The study provides a theory that changes in possible neurophysiologic or mechanical constraints on postural control follow cerebral concussions. The authors suggest a technology that measures subtle changes in postural control might improve return-to-play decisions. [6]
Patients rarely report long-term symptoms of concussion. [7] Athletic trainers report that symptoms and effects of concussion resolve within seven to 10 days. [8] It is common that patients return to athletic activities and unrestricted activities of daily living before resolution of MTBI symptoms. [9] Other studies indicate that concussion symptoms may persist for a longer time than reported by patients. It has been demonstrated that MTBI patients walked slower and allowed a reduced amount of postural control within the initial 48 hours post-trauma. When tested with challenges, such as obstacle crossing two weeks post-trauma, the patients demonstrated motor dysfunction and less control of medio-lateral motion of their center of mass. These motor dysfunction findings do not support the theory that patients with MTBI return to normal motor functioning within two weeks. [10]
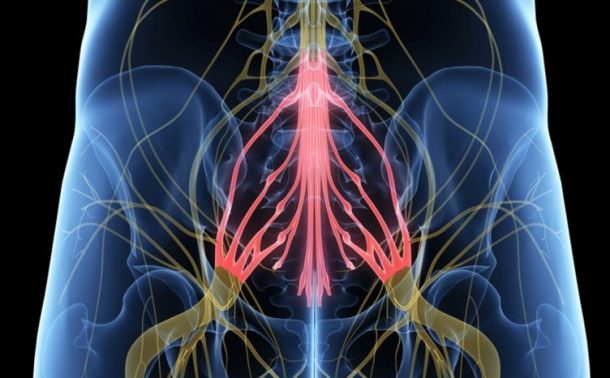
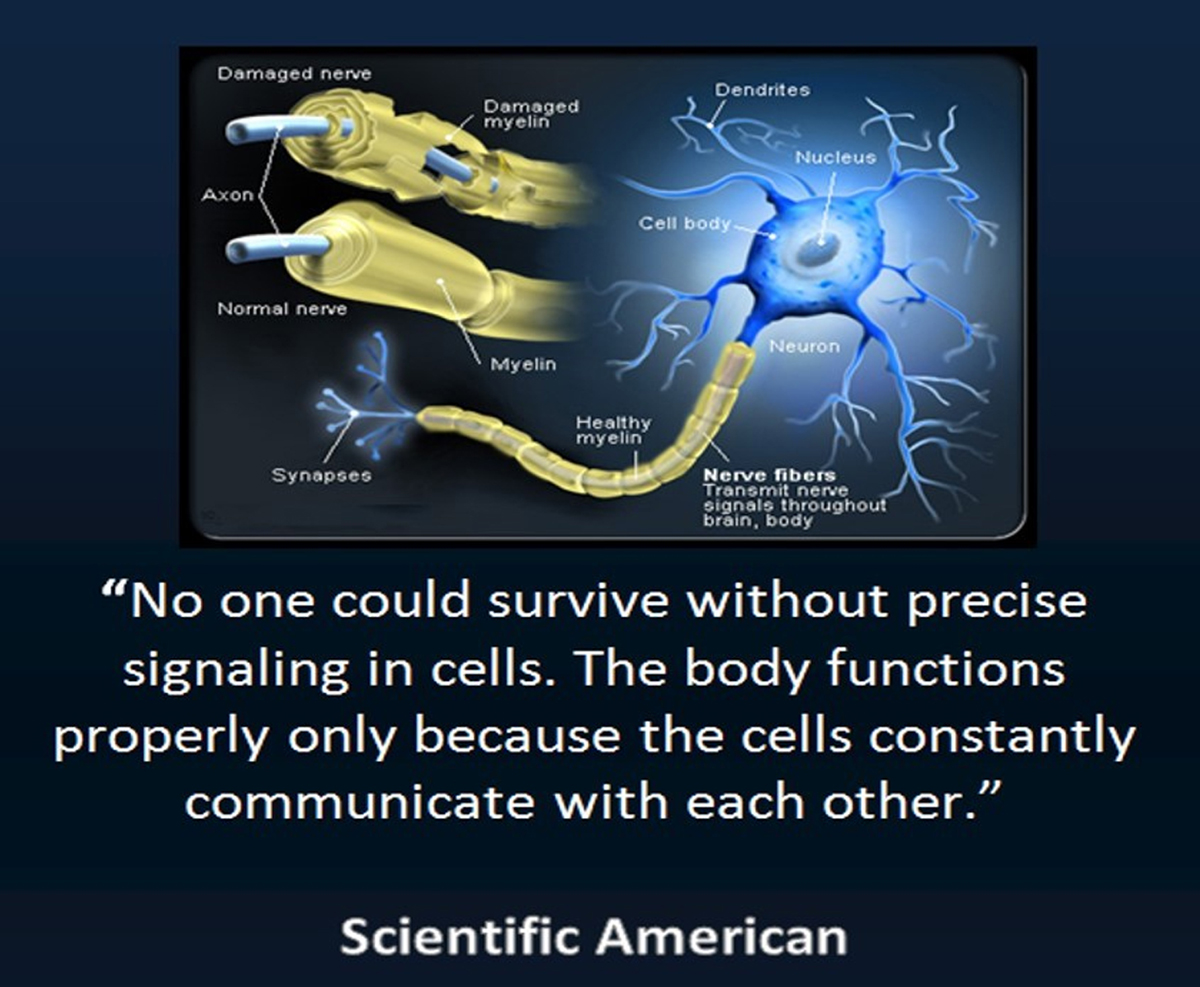
It has been reported that impact acceleration to the head causes traumatic brain injuries (TBI) with damage to the white matter tracts composed of long axons traversing the brain. The acceleration-deceleration shearing forces generated by motor vehicle accidents and the rotational shearing forces generated with boxing, most especially the uppercut, cause diffuse axonal injury. [11] The initial response to mechanical axonal injury is reversible. Incomplete clinical evaluation of the involved white matter and early return to unrestricted activities may lead to secondary insults and irreversible axonal fragmentation. [12] Studies demonstrate that ultra-high field MRI [13] and diffusion tensor imaging MRI reveal microstructural tears of axons and small vessels. [14]
Brain Protection
About 35 years ago, neurologists called for a ban on boxing in order to reduce the incidence of traumatic brain injuries. [15] Since that time, neurologists have changed their position and embrace the opportunity to reduce TBI as sports neurologists with current guidelines that attempt to answer the following questions. [16]
- For athletes, what factors increase or decrease concussion risk?
- For athletes suspected of having a concussion, what diagnostic tools are useful in identifying those with concussion?
- For athletes with a concussion, what clinical factors are useful in identifying those at increased risk for severe or prolonged early post-concussion impairments, neurologic catastrophe, recurrent concussions or late neurobehavioral impairment?
- For athletes with a concussion, what interventions enhance recovery, reduce the risk of recurrent concussion or diminish late neurobehavioral impairment? Sports neurologists now believe concussion in sports is a public health problem that necessitates their educating athletes in brain protection based on the most current evidence. [17]
Concussion/MTBI and the Team Physician
A consensus statement by the American College of Sports Medicine attempts to assist the team physician in providing optimal medical care for athletes who have experienced a concussion. To accomplish the goal, the college suggests that all team physicians should have knowledge of and be involved with the following: [18]
- Epidemiology
- Pathophysiology
- Gameday evaluation and treatment
- Post-gameday evaluation and treatment
- Diagnostic imaging
- Management principles
- Return-to-play
- Complications of concussion
- Prevention
American Medical Society for Sports Medicine Position Statement: Concussion in Sport
The purposes of this statement are to provide an evidence-based, best practices summary to assist physicians with the evaluation and management of sports concussion and to establish the level of evidence, knowledge gaps and areas requiring additional research. Interestingly, the society stated that the ideal care of athletes with sports concussion should be performed by health care professionals with specific training and experience in the assessment and management of concussion. Hence, the sports medicine position intends to assist sports medicine physicians, other physicians and health care professionals in the care of patients with sports concussion. [19] This integrative mentality appears to support the National Prevention Strategy: America’s Plan for Better Health and Wellness recommendation to enhance coordination and integration of clinical, behavioral and complementary health strategies. [20]
Integrated health care describes a coordinated system in which health care professionals are educated about each other’s work and collaborate with one another and with their patients to achieve optimal patient well-being.
Discussion
Injured individuals are usually not aware of their MTBI and often do not seek care. In order to improve the treatment of these patients, all health care providers should become more aware of best practices and evidence-based care of MTBI and concussion. All health providers treating athletes should become familiar with the guidelines offered in this article.
It is important that any health care provider evaluating a brain-injured athlete, worker or patient be able to determine the level of consciousness and gauge the severity of an acute brain injury. The treatment of MTBI/concussion should be performed by health care professionals with specific training, experience and credentialing in the assessment and management of concussion. Chiropractic physicians should pursue education and credentialing offered online by HEADS UP, Brainline.org and BrainlineMilitary.org. Chiropractic colleges should provide postgraduate education and training, preparing chiropractic physicians to evaluate and manage patients with concussions and mild traumatic brain injuries.
Endnotes
- Harmon KG, Drezner JA, Gammons M, Guskiewicz KM, et al.
American Medical Society for Sports Medicine position statement: concussion in sport.
See comment in PubMed Commons below Br J Sports Med. 2013 Jan; 47(1):15-26. - National Center for Injury Prevention and Control.
Report to Congress on Mild Traumatic Brain Injury in the United States:
Steps to Prevent a Serious Public Health Problem. Atlanta, GA:
Centers for Disease Control and Prevention; 2003. - David Martinez.
Research & Science: Bloodless Concussion: _e Misunderstood Injury.
J Amer Chiropr Assoc 2011 Sept- Oct; 48(7):16-39. - Teasdale G, Jennett B,
Lancet (ii) 81-83, 1974. - McCrory P, Meeuwisse W, Aubry M, Cantu B, et al.
Consensus Statement on Concussion in Sport—the 4th International Conference on Concussion in Sport.
Held in Zurich, Nov. 2012.
Clin J Sport Med Volume 23, Number 2, March 2013. - Cavanaugh JT. Guskiewicz KM; Giuliani C; Marshall S; Mercer VS; Stergiou N.
Recovery of Postural Control After Cerebral Concussion: New Insights Using Approximate Entropy.
Journal of Athletic Training 2006; 41(3):305–313. - Krauss JK, Tränkle R, and Kopp KH:
Posttraumatic movement disorders after moderate or mild head injury.
Mov Disord 1997, 12(3):428-431. - Covassin T, Elbin III R, and Stiller-Ostrowski JL.
Current Sport-Related Concussion Teaching and Clinical Practices of Sports Medicine Professionals.
ATC Journal of Athletic Training 2009;44(4):400–404. - Parker TM, Osternig LR, van Donkelaar P, Chou LS:
Gait stability following concussion.
Med Sci Sports Exerc 2006, 38(6):1032-1040. - Catena RD, van Donkelaar P and Chou L.
Different gait tasks distinguish immediate vs. long-term effects of concussion on balance control.
Journal of NeuroEngineering and Rehabilitation 2009, 6:25. - Adams JH, Doyle D, Ford I, Gennarelli TA, Graham DI, McLellan DR.
Diffuse axonal injury in head injury: definition, diagnosis and grading.
Histopathology. 1989; 15: 49–59. - Armstrong RC, Mierzwa AJ, Marion CM, Sullivan GM.
White matter involvement after TBI: Clues to axon and myelin repair capacity.
See comment in PubMed Commons below
Exp Neurol. 2015 Feb 16. Pii: S0014-4886(15)00034-5. - Moenninghoff C, Kraff O, Maderwald S, Umutlu L, et al.
Diffuse Axonal Injury at Ultra-High Field MRI.
PLOS ONE. March 20, 2015. - Alexander AL, Lee JE, Lazar M, and Field AS.
Diffusion Tensor Imaging of the Brain.
Neurotherapeutics. 2007 Jul; 4(3): 316–329. - American Academy of Neurology, 1983–1985 Membership Directory.
Minneapolis, MN: American Academy of Neurology; XIV, XX; 1984. - Alessi AG, Mayer T and Smith D.
Protecting the brain in sports: What do we really know?
American Academy of Neurology.
Position Statement on Sports Concussion. Oct. 2010. - Giza CC, Kutcher JS, Ashwal S, Barth J, et al.
Summary of evidence-based guideline update: Evaluation and management of concussion in sports.
Report of the Guideline Development Subcommittee of the American Academy of Neurology.
Neurology 2013. - Concussion (Mild Traumatic Brain Injury) and the Team Physician:
Consensus Statement.
Med Sci Sports Exerc. 2006 Feb; 38(2):395-9. - Harmon KG1, Drezner JA, Gammons M, Guskiewicz KM, et al.
See comment in PubMed Commons below
Br J Sports Med. 2013 Jan; 47(1):15-26. - National Prevention Council, National Prevention Strategy,
Washington, DC: U.S. Department of Health and Human Services,
Office of the Surgeon General, 2011.
Online Traumatic Brain Injury Resources
By Shereen K. Lehman, DC, DABCI and James J. Lehman, DC, FACO
There’s always more to learn about traumatic brain injuries, and the body of research is constantly growing. These three websites offer excellent resources for doctors, patients, coaches and community members.
Here’s how to stay up-to-date with the latest news, study traumatic brain injury (TBI) in depth and even earn a few continuing education units.
HEADS UP
HEADS UP (www.cdc.gov/headsup/about/index.html) includes a series of educational initiatives, developed by the Centers for Disease Control and Prevention. The goal of HEADS UP is to protect children and teens from concussions and other serious brain injuries “by raising awareness, enhancing knowledge and informing action to improve prevention, recognition and response to concussion and other serious brain injuries.” [1]
The website has materials for health care professionals to learn more about diagnosing and managing concussions, including online concussion training, diagnostic and assessment tools, patient handouts and guidelines for determining when it’s safe to send student-athletes back on the field or court.
The online training program covers current research on what happens to the brain after a concussion and examines risk factors for kids and concussions. It also focuses on prevention of TBI and includes a “5-Step Return to Play” progression designed to help you decide when and how students return to play. Continuing education credits are available upon completion of the course.
In addition to the wealth of resources for the health professional, HEADS UP has sections specifically created for parents, coaches and athletic directors, teachers and school administrators, and even a section on sports concussion policies and laws.
BRAINLINE.ORG
BrainLine.org (www.brainline.org) is an awardwinning national multimedia project that offers information and resources about preventing, treating and living with traumatic brain injury. [2] The website is produced by WETA, a public TV and radio station in Washington, D.C., along with a number of partners.
The comprehensive website is broken down into four sections: basic TBI information, resources for professionals, help for patients and even more help for friends and family members. Resources include videos, articles, webcasts, audio, interactive media and slide shows.
BrainLine.org also offers an Ask the Expert series featuring new questions and answers each month about traumatic brain injury. In addition, there are descriptions of smartphone apps that may help TBI patients live with their condition.
BRAINLINEMILITARY.ORG
Brain injuries are some of the most common injuries suffered during the wars in Afghanistan and Iraq. TBI may be accompanied by post-traumatic stress and other conditions unique to the military, so BrainLine.org offers a secondary site called BrainLineMilitary.org (www.brainlinemilitary.org).
The website provides military-specific information and resources on traumatic brain injury to veterans; service members in the Army, Navy, Air Force, Marines, National Guard and Reserves; and their families. [3] The Bob Woodruff Foundation and Newman’s Own Foundation partially support the website.
Like its parent website, BrainLineMilitary.org has videos, webcasts, articles, personal stories, research briefs and current news. In addition, BrainLineMilitary.org offers online courses for health care providers, including how to diagnose and treat concussion and mild TBI in service members and veterans and understanding deployment-related TBI and co-occurring conditions.
Endnotes
- Centers for Disease Control and Prevention.
HEADS UP to Health Care Providers.
www.cdc.gov/headsup/providers/index.html - BrainLine.org.
About Us.
www.brainline.org/function_ pages/about.html - BrainLineMilitary.org.
About Us.
www.brainlinemilitary.org/sub_pages/mil_about_us.php



Lots of great information here. Glad that there’s a resource out there that lists out everything about MTBI like this. Thanks so much for sharing!