Epidural Corticosteroids for Sciatica
SOURCE: Dynamic Chiropractic
By Deborah Pate, DC, DACBR
Use of epidural steroid injections has increased dramatically in recent years, despite the fact that studies have failed to demonstrate evidence this procedure is clinically helpful (while other studies suggest it may actually be dangerous).
Considering that lack of evidence – not to mention the terrible 2012 outbreak of fungal meningitis / infections [see sidebar] caused by contaminated vials used for epidural corticosteroid injections – it is prudent at least to take a critical look at this procedure, particularly as it relates to conditions doctors of chiropractic treat.
Steroid Injections for Sciatica: Small, Short-Term Relief Only
In a recent meta-analysis of 23 randomized trials involving more than 2,000 patients in which epidural steroid injections were compared with placebo for sciatica, epidural steroid injections produced small, statistically insignificant short-term improvements in leg pain and disability (but not less back pain) compared to placebo. This improvement also was only over a short period of time – two weeks to three months. Beyond 12 months, there was no significant difference between groups. [1]
Side Effects Including Skeletal Deterioration, Fracture Risk
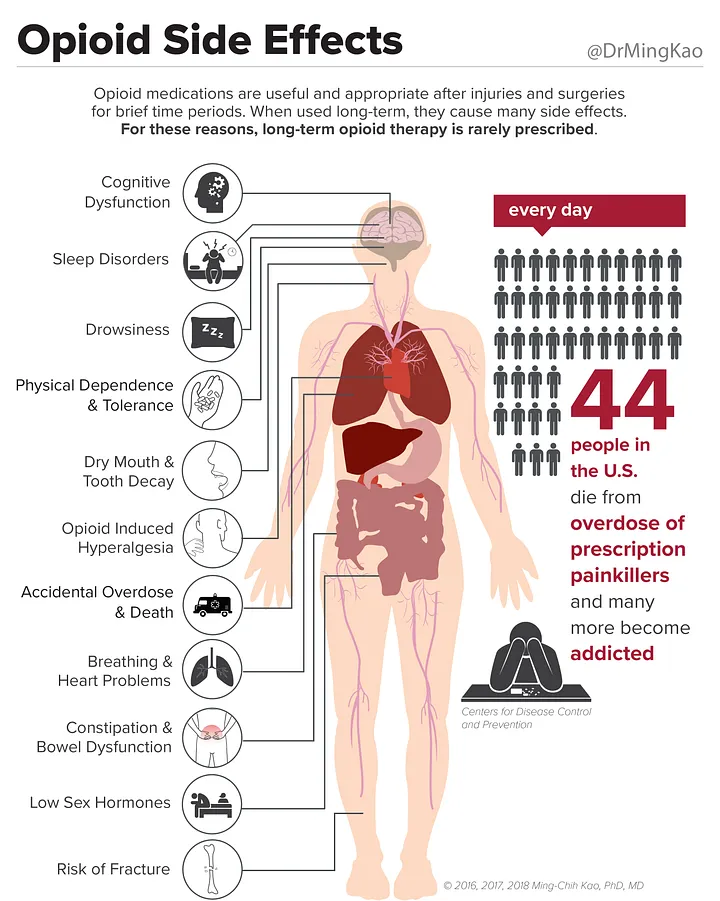
Besides infection, there are other side effects associated with epidural steroid injections: bleeding, nerve damage and dural puncture. Then there are side effects associated with the steroid medication, which include the following: a transient decrease in immunity, high blood sugar, stomach ulcers, avascular necrosis (mainly in the hip joint), cataracts and increased risk of fracture.
| Tainted Steroid Injections: The Framingham Outbreak In September 2012, the CDC and the FDA began investigating a multistate outbreak of fungal meningitis and other infections among patients who had received contaminated steroid injections. The contaminated vials were tracked back to a New England compounding center in Framingham, Mass.
The cases included fungal meningitis; localized spinal or paraspinal infections, including epidural abscess, basilar stroke, vertebral osteomeylitis and arachnoiditis; and infections associated with injection in a peripheral joint space such as the knee, shoulder or ankle. Ultimately, the outbreak resulted in 751 cases and 64 deaths in more than 20 states. |
This last complication is certainly not emphasized in clinical circles. Therapeutic steroids may reduce pain, however the use of steroid injections seem to promote deterioration of skeletal quality, which is not surprising since other forms of steroid medication have long been associated with osteoporosis.
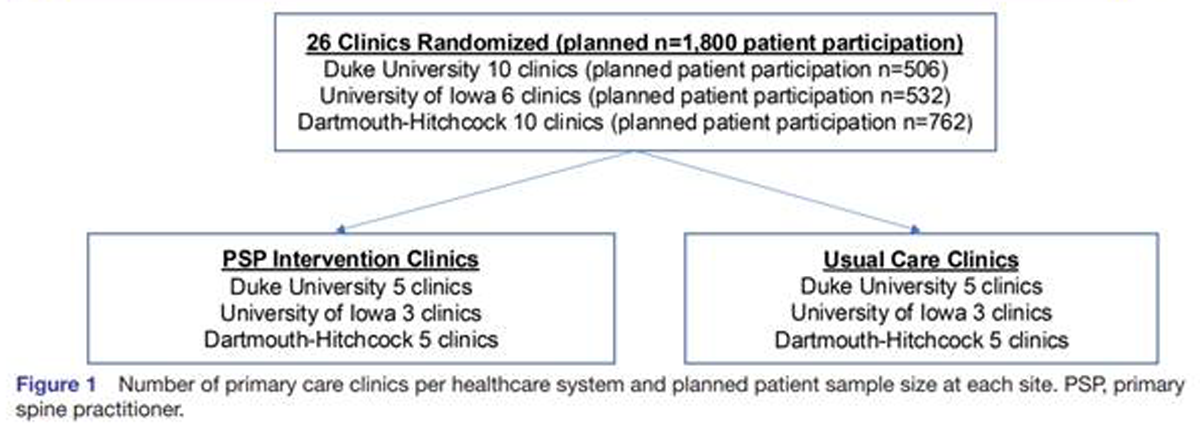
A retrospective study published in the Journal of Bone and Joint Surgery looked at lumbar epidural steroid injection (LESI), and the potential impact on bone fragility and vertebral fractures (spinal fractures). Researchers identified a total of 50,345 patients who had medical diagnosis codes involving the spine; within that group, a total of 3,415 patients had received at least one LESI.
Three thousand patients were randomly selected from the 3,415 injected population and 3,000 additional patients were selected from the non-injected group as a control group. There was no significant difference between the injected and non-injected groups with respect to age, sex, race, hyperthyroidism or corticosteroid use.
When incidence of vertebral fractures was assessed, researchers discovered that an increasing number of injections was associated with an increasing likelihood of fractures, and each successive injection increased the risk of spinal fracture by 21 percent. [2] Based on this evidence, LESIs clearly exacerbate skeletal fragility. They promote deterioration of skeletal quality similar to the use of exogenous steroids, which is the leading cause of secondary osteoporosis. In fact, the rate of vertebral fracture following epidural steroid injections may be underestimated.
Both European and American guidelines, based on systemic reviews, conclude that epidural corticosteroid injections may offer temporary relief of sciatica, but do not reduce the rate of subsequent surgery. [3] This conclusion is based on multiple randomized trials comparing epidural steroid injections with placebo injections, and monitoring of subsequent surgery rates. [4] Facet joint injections with corticosteroids seem no more effective than saline injections. [5, 6]
Rising Costs, Limited Benefits
Despite the limited benefits of epidural injections, Medicare claims show a 271 percent increase during a recent seven-year interval.7 Earlier Medicare claims analyses also demonstrated rapid increases in spinal injection rates. For patients with axial back pain without sciatica, there is no evidence of benefit from spinal injections; however, many injections given to patients in the Medicare population seem to be for axial back pain alone. [7]
Charges per injection have risen 100 percent during the past decade (after inflation), and the combination of increasing rates and charges has resulted in a 629 percent increase in fees for spinal injections. [7] Yet during this time, the Medicare population increased by only 12 percent.
It all begs the question: Why such a huge increase in the use of a procedure that has limited benefit? Patients need to be informed about treatment options including the best evidence for effectiveness, uncertainties and risks, so they can take an expanded role in decision-making.
Clinical Pearls
- Epidural steroid injections have little clinical benefit (short or long term) and are associated with significant risks.
- Steroid injections cause deterioration of bone quality, elevating the risk of spinal fracture.
- Use of epidural steroid injections has increased dramatically despite lack of evidence to justify the procedure.
References
- Pinto RZ, et al.
Epidural corticosteroid injections in the management of sciatica:
A systematic review and meta-analysis.
Ann Intern Med, 2012 Nov 13; [e-pub ahead of print]. - Mandel S, Schilling J, Peterson E, et al.
A retrospective analysis of vertebral body fractures following
epidural steroid injections.
J Bone & Joint Surg, 2013 Jun;95(11):961-964. - Armon C, Argoff CE, Samuels J, Backonja M.
Assessment: use of epidural steroid injections to treat radicular
lumbosacral pain. Report of the Therapeutics and Technology Assessment
Subcommittee of the American Academy of Neurology.
Neurology, 2007;68:723-9. - Arden NK, Price C, Reading I, et al.
A multicentre randomized controlled trial of epidural corticosteroid
injections for sciatica: the WEST study.
Rheumatol,2005;44:1399-406. - Airaksinen O, Brox JI, Cedraschi C, et al.
European guidelines for the management of
chronic nonspecific low back pain.
Eur Spine J, 2006;15(Suppl 2):S192–S300. - Chou R, Rosenquist R, Loeser J.
ACP-APS Guidelines for Surgical and Interventional Procedures
for Chronic Low Back Pain.
Presented at Symposium 312 of the American Pain Society’s 27th
Annual Scientific Meeting, Tampa, Fla., May 8, 2008. - Friedly J, Chan L, Deyo R.
Increases in lumbosacral injections in the Medicare population: 1994–2001.
Spine, 2007;32:1754-60
Deborah Pate is a licensed chiropractor and a diplomate of the American Chiropractic Board of Radiology. A 1982 graduate of National College of Chiropractic, she was the first chiropractor accepted into a fellowship in osteoradiology at the medical center of the University of California, at San Diego.




Leave A Comment