Startling New Study Reveals That Back Surgery Fails 74% of the Time
A Chiro.Org Editorial
SOURCE: Spine (Phila Pa 1976) 2011 (Feb 15); 36 (4): 320–331
Nguyen TH, Randolph DC, Talmage J, Succop P, Travis R.
From the Division of Epidemiology and Biostatistics,
Department of Environmental Health,
University of Cincinnati College of Medicine,
Milford, OH
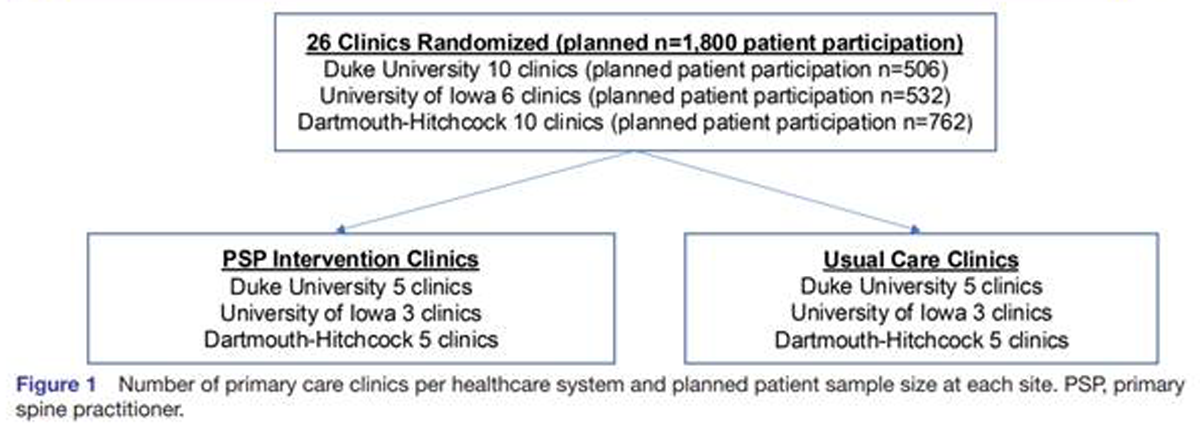
Researchers reviewed records from 1,450 patients in the Ohio Bureau of Workers’ Compensation database who had diagnoses of disc degeneration, disc herniation or radiculopathy, a nerve condition that causes tingling and weakness of the limbs. Half of the patients had surgery to fuse two or more vertebrae in hopes of curing low back pain. The other half had no surgery, even though they had comparable diagnoses.
After two years, only 26 percent of those who had surgery had actually returned to work. That’s compared to 67 percent of patients who didn’t have the surgery, even though they had the same exact diagnosis.
That translates to a resounding 74% failure rate! It also suggests that you have a 257% better chance of returning to work IF YOU AVOID SURGERY in the first place!
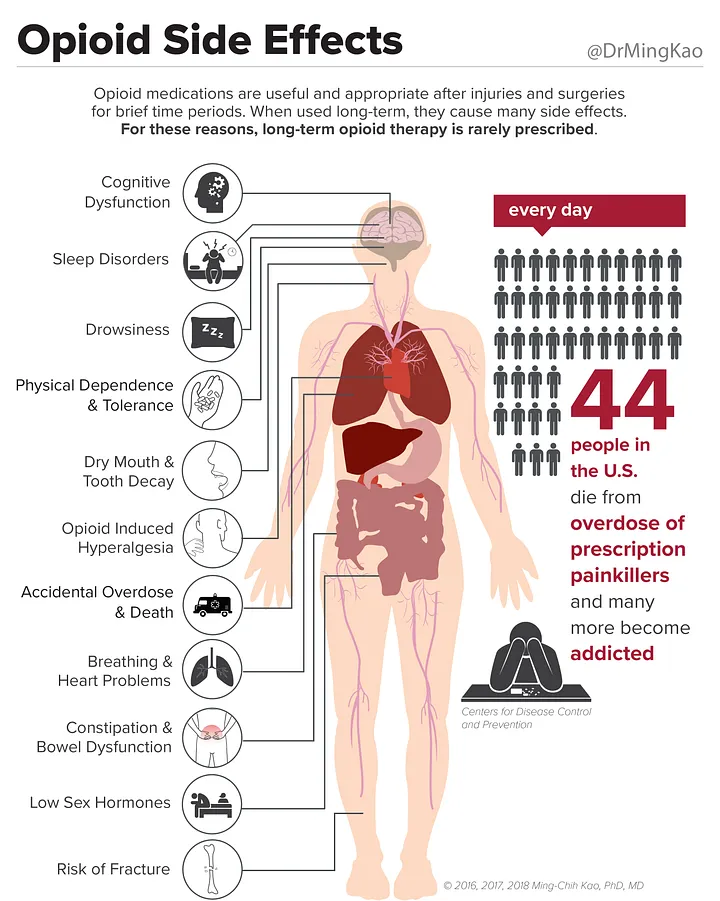
In another troubling finding, the researchers determined that there was a 41 percent increase in the use of painkillers, particularly opiates, in those who had the surgery. Last year we reported that deaths from addictive painkillers has doubled in the last 10 years. [6]
“The study [1] provides clear evidence that for many patients, fusion surgeries designed to alleviate pain from degenerating discs doesn’t work”, says the study’s lead author Dr. Trang Nguyen, a researcher at the University of Cincinnati College of Medicine. [2]
Just a month after back surgery, Nancy Scatena was once again in excruciating pain. The medications her doctor prescribed barely took the edge off the unrelenting back aches and searing jolts down her left leg. “The pain just kept intensifying,” says the 52-year-old Scottsdale, Ariz., woman who suffers from spinal stenosis, a narrowing of the chanel through which spinal nerves pass. “I was suicidal.”
Finally, Scatena made an appointment with another surgeon, one whom friends had called a “miracle worker.” The new doctor assured her that this second operation would fix everything, and in the pain-free weeks following an operation to fuse two of her vertebrae it seemed that he was right. But then the pain came roaring back.
Experts estimate that nearly 600,000 Americans opt for back operations each year. But for many like Scatena, surgery is just an empty promise, say pain management experts, and even some surgeons.
This new study in the journal Spine [4] shows, that in many cases, surgery can backfire, leaving patients in more pain..
27 Million Adults With Back Problems
A recent report by the Agency for Healthcare Research and Quality, a federal organization, found that in 2007, twenty-seven million adults reported back problems, with $30.3 billion spent on treatments to ease the pain. While some of that money is spent on physical therapy, pain management, chiropractor visits, and other non invasive therapies, a big chunk pays for spine surgeries.
Complicated spine surgeries that involve fusing two or more vertebrae are on the rise.
In just 15 years, there was an eight-fold increase in this type of operation, according to a study published in Spine in July. That has some surgeons and public health experts concerned. [4]
You may also want to review the recently published
European Guidelines for the Management of Acute and Chronic Nonspecific Low Back Pain, because it states:
“Surgery for non-specific CLBP cannot be recommended unless 2 years of all other recommended conservative treatments — including multidisciplinary approaches with combined programs of cognitive intervention and exercises — have failed”.
This study re-confirms the findings of the UK BEAM Trial, published in the British Medical Journal in 2004. [5] Those authors stated:
“Manipulation, with or without exercise, improved symptoms more than best care (medical care) alone after three and 12 months. However, analysis of the cost utility of different strategies shows that manipulation alone probably gives better value for money than manipulation followed by exercise” (page 1381).
You may also want to read these 3 recent Editorials:
Why Do Spinal Surgery Rates Continue To Rise?
Chiro.Org Blog ~ April 10th, 2010New Study Finds Chiropractic Care Superior to Family Physician-directed Usual Care
Chiro.Org Blog ~ October 7th, 2010If Not Chiropractic Care, Then What’s Your Alternative?
Chiro.Org Blog ~ September 25th, 2010
REFERENCES:
- Long-term Outcomes of Lumbar Fusion Among Workers’ Compensation Subjects:
An Historical Cohort Study
Spine (Phila Pa 1976) 2011 (Feb 15); 36 (4): 320–331 - Study Says Back Surgery Often Makes Things Worse
The Daily Hit ~ Oct 14, 2010 - Back Surgery May Backfire On Patients In Pain
MSNBC.com ~ Oct 14, 2010 - Why Do Spinal Surgery Rates Continue To Rise?
Chiro.Org Blog Editorial ~ April 10th, 2010 - Findings from the: “United Kingdom Back Pain Exercise and Manipulation
(UK BEAM) Randomised Trial”
British Medical Journal 2004 (Dec 11); 329 (7479): 1377 - Painkiller Deaths Double In Ontario
Chiro.Org Blog ~ 12-08-2009




These ever increasing # of surgeries are a result of the tunnel vision within current medical thought. They look at the area of problem, but don’t take in to consideration the total functional neuro-biomechanical picture of the patient. They concentrate on the “tree” and totally forget to look at the “forest” it grows in. If you don’t address the fundamental underlying biomechanical faults, surgery will almost always fail
I’ve seen the good, the bad and the ugly regarding patients that have had lowback surgery. Specifically, fusions, laminectomies and microdiskectomy. I’m personally not going to be black and white when it comes to lowback surgery. I’ve had/see patients that have had good results. When it comes to “failures” there are many variables to consider……one being a person’s perceived/tolerance of pain. Some of the said microdiskectomy patients were in a lot of pain and couldn’t afford the time/employment compensation to be out of work. Therefore diagnosis/evaluation is key when determining the best candidates for lowback surgery. It’s my opinion, proper diagnosis/evaluation of the patient and their respective advanced imaging is an area of concern. Of course there many other variables to consider but that’s difficult. I believe conservative chiroractic care along with rational pain control medication should be a first choice for some of these potential lowback surgery patients.
Couldn’t agree with Dr. Rich anymore!
Good post that brings what many in practice see all of the time. I’m fortunate to work with a Neurosurgeon that knows this and refers to chiropractors regularly.
These are the facts people need to know. Surgery should only be used as a last resort. By educating the public, chiropractors can help save many people from the misery that many of these surgeries can cause.
74% is a staggering number. I recommend exhausting any possible non invasive option first, which always includes chiropractic. Surgery should only be an option if all else fails to stabilize the spine. Knowledge is power. Get the facts first before jumping into a procedure that could potentially cause more harm than good.
[…] This post was mentioned on Twitter by Dr. Stephanie Maj, Dr. David H. Mruz, Sally Cutler, Drs. Maj & Miller, Karla Miller and others. Karla Miller said: Researchers reviewed 1,450 patients & after two years, 26 % of those who had surgery had returned to work. Chiro FIRST! http://bit.ly/9vcdet […]
[…] “The study [1] provides clear evidence that for many patients, fusion surgeries designed to alleviate pain from degenerating discs don’t work”, says the study’s lead author Dr. Trang Nguyen, a researcher at the University of Cincinnati College of Medicine. [2] (Read the full article here.) […]
It’s interesting how there is even a diagnosis that they’ve created for cases such as this (Failed Back Syndrome or Failed Back Surgery Syndrome). Back in 2001, the problem was brought to light by Hubert L. Rosomoff, MD, when he realized that, after two weeks of rehabilitation, his back patients no longer required surgery.
He went on record stating, “Following this kind of concept you can eliminate 99 percent of the surgical cases. In fact, the incidence of surgery if one really looks at this appropriately is one in 500.”
He also went on to say that “Backs don’t fail people, Doctors do!”.
All surgery carries with it a significant degree of patient risk but back surgery fails most of the time. Not only does the surgery not alleviate the problem of back pain, it often creates even greater problems for the patient. And the insurance companies are still paying for this?
Seattle,
One only need review members of the Advisory Boards for any insurance carrier to see that MDs dominate and dictate policy decisions, such as which services are covered (and it’s ALWAYS medicine, surgery) and which aren’t (sometimes it’s chiropractic).
What boggles the mind is how often people end up getting a second, third, or fourth back surgery. My question is, if you need your appendix out, how many times do you need that surgery?
If surgery ACTUALLY works (or was appropriate), then just one should do it, right??? Evidently, that’s not the case.
The simple truth is that surgical disruption of discs, or worse yet spinal fusions, cause instability of the spine, that invariably causes the decline of segments immediately above or below where the surgery occurred. As evidence-based approaches start looking at the long-term effects of spinal surgery, it will become even more obvious that surgery is a very bad choice, except for extruded nucleus pulposus (free fragments in the canal or at the nerve roots). That should be considered a “medical emergency” and should be removed immediately.
It’s nice to see that what i have been teaching for the last decade now has rock solid evidence. Too many of my patients have gone that route. Now I have more conviction in trying to sway them from going down this path.
Wow…I understood that back surgery failed (mechanically) long-term, but this is staggering to see this high rate of failure. Time to print out that reference and send out a Tweet – thanks for sharing!
I can see Frank’s interpretation as more than likely pretty right on, I and can add that I recently heard a work comp guru speak. This person mentioned that many small to medium sized west coast hospitals make 100K+ per back surgery or (BS)and usually do 50 to 70 per month. If you add the numbers up you might see why the amount of surgeries, regardless of work comp, might not be going down anytime soon-regardless of the studies etc.
It makes sense that good patient education is a good place to start. Perhaps even a mailing campaign to the GP’s in your area educating them with this study and other pro chiropractic studies already mentioned. Probably a good return on investment for the patients, their MD’s and potential referrals to you.
It appears that this type of information/studies has been around for quite some time. I believe, I remember hearing that the Texas Back Institute did a study in the late 80’s and determined that less than 2% of all back surgeries (BS)were necessary. I have also heard plenty of failed surgery stats over the years, including that only 37% of the hot new laser surgeries are effective. You even have to pay cash for those- insurance does not seem to want to recognize them, last I heard. Kind of like Non-Surgical Spinal Decompression that seems have a much higher success rate with a relatively low comparison cost and little to no complications or recovery time.
Since the 80’s, even after all the compelling negative literature on BS, it seems that the number of back surgeries are up: the number of failed back surgeries are up and back surgery Profits are up.
Perhaps we can just call it Quantitative Easing III-BS with no accountability necessary?
Thanks Mark.
It’s the classic case of the fox minding the hen house.
I called an Insurance Company to get a new patient’s benefits, and the agent droned on that for medical benefits, the deductible was 300 and co-insurance was at 70%
I said “That’s fine, but I’m a Chiropactor”
The agent brightened right up and said:
“Oh, for chiropractic, deductible is only 200, and the co-insurance pays at 80%!”
Imagine that, experiencing an Insurer preferentially (and financially) steering clients towards chiropractic care!
And when you look at the recent posts we’ve made, about the superiority and cost-effectiveness of chiropractic, it’s only a matter of time before more Insurers do the same thing. It makes sense (and dollars saved!).
Frank,
That IS encouraging! Hopefully it is a sign that things are starting to change, and more insurers will encourage chiropractic.
Thanks for the brilliant information – anyone considering back surgery needs to know
I have seen (and I’m sure we all have) so many cases where a patient was in so much chronic pain after a lumbar fusion because he/she had traded the spinal pain for semi-permanent muscle spasm. The failure rate looked to be about 74% to me — now it is verified.
There was a news story this morning on doctors who are investing in a company that makes hardware for a particular spinal surgery performing it more often than is necessary. Hmmmm….
RESPONSE from Frank
We posted a review titled “Why Do Spinal Surgery Rates Continue To Rise?” last April after the New York Times published an article that stated:
Those concerns are now heightened by a growing trend among some surgeons to profit in yet another way — by investing in companies that make screws and other hardware they install.
My concern?
Now we have to wonder if the orthopedist might be motivated to install 6 of those $1000 screws to your spine just because they are a stockholder of a lucrative medical device manufacturing company. UGH!
Everyone rolls their eyes when they hear about the $400 ashtrays in defense contracts…but what about these $1000 screws? God help us!
I am looking for the 76% failure study and can’t seem to find it. Some assistance would be greatly appreciated. If anyone could point me to a way to get a copy for patients it would be nice.
Thanks. Mark
RESPONSE from Frank:
It was 74%, but the intro paragraph mentions that number, and it’s the 1st reference, listed towards the bottom of the page. Invariably all those are hot-linked directly to the article…and Full-Text when I can get to it.
The author states: “Two years after fusion surgery, 26% (n = 188) of fusion cases had RTW (return to work)“, so that translates to 74% who are still not to work after 2 YEARS! That’s the failure this article discusses.
That is an amazing statistic! I wonder why so many people still see surgery as the “fix” for their problem. For most people, it should only be used after all else has failed.
I’ve rarely heard positive reviews after back surgeries. Medicine has a ways to go before people are going to feel comfortable going under the knife in this regard.
RESPONSE from Frank
I’ve heard wonderful commentary from folks shortly after decompression surgery. The problem is that they have to fuse the segment, and that destabilizes the whole spinal region, causing problems above and below the fused segment, or what they call “failed back syndrome”, leading to additional surgeries.
That makes no more sense than simply giving them morphine. Surgeries appear to NOT be corrective. That’s why I love the McKenzie protocol for disc. It’s simple, elegant and virtually 100% effective for improving disc derangement.
I JUST read a review of this article on another web site, in which an MD sniffed as she stated that this study had no value since it was about “workers”, and “we all know” that they don’t really want to go back to work. Whooo-eee, that’s harsh!
What she conveniently (or ignorantly?) ignored is that BOTH groups in this article are “workers”, and the evidence was:
So… if her “opinion” was actually grounded in fact (rather than expressing self-deceptive bias), wouldn’t the “workers” that did not get the surgery be just as likely to be sitting at home, watching Oprah?
One would think. Anyone who has been in practice for a year knows that these surgeries really hurt many patients.
Very startling numbers – It’s great to have research and blog posts like this to share with friends, family and patients.