Why Do Spinal Surgery Rates Continue To Rise?
A Chiro.Org Editorial
First, let’s review some history. In 1974, the Congressional Committee on Interstate and Foreign Commerce held hearings on unnecessary surgery. Their findings from the First Surgical Second Opinion Program found that 17.6% of recommendations for surgery were not confirmed. The House Subcommittee on Oversight and Investigations extrapolated these figures to estimate that, on a nationwide basis, there were 2.4 million unnecessary surgeries performed every year, resulting in 11,900 deaths, at an annual cost of $3.9 billion. [1]
With the total number of lower back surgeries having been estimated in 1995 to exceed 250,000 in the U.S., at a hospital cost of $11,000 per patient. [2] This could suggest that the total number of unnecessary back surgeries each year in the U.S. could be 44,000, costing as much as $484 million. [3]
So, the first risk of spinal surgery is that it may not be necessary.
A most-recent review suggests that:
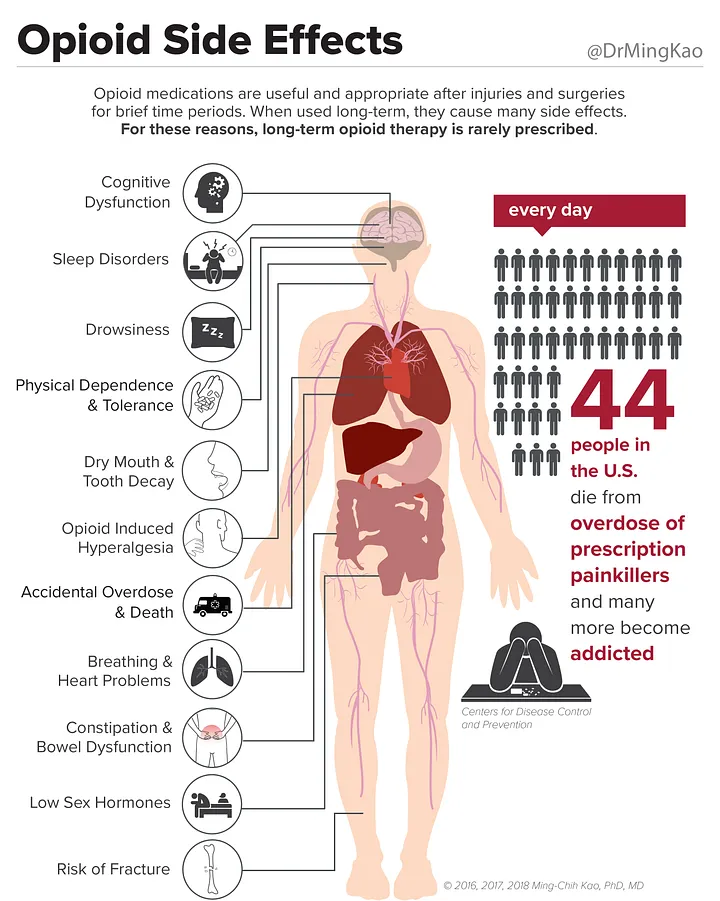
The next set of risks include:
- a 2.1% chance of a serious adverse drug reaction. [4]
- a 5-6% chance of acquiring a nosocomial infection [5]
- a 4-36% chance of having an iatrogenic injury (medical error or adverse drug reactions). [6]
- a 17% chance of a procedure error. [7]
AND… as few as 3%, and no more than 20% of iatrogenic injuries are EVER reported! Yipes! [8]
That takes all the fun out of being a statistic, doesn’t it?
This September 2006 article from the Journal of the American Academy of Orthopedic Surgeons says it all:
“Failed back surgery syndrome is a common problem with enormous costs to patients, insurers, and society. The etiology of failed back surgery can be poor patient selection, incorrect diagnosis, suboptimal selection of surgery, poor technique, failure to achieve surgical goals, and/or recurrent pathology.” [9]
That is straight from the horse’s mouth.
Other testimony is equally disturbing:
A recent definitive review of the biomedical literature and government health statistics revealed that American medicine frequently causes more harm than good. The number of unnecessary medical and surgical procedures performed annually is 7.5 million. The number of people exposed to unnecessary hospitalization annually is 8.9 million. [8]
A 1987 JAMA study found the following significant levels of inappropriate surgery:
- 17% of cases for coronary angiography,
- 32% for carotid endarterectomy, and
- 17% for upper gastrointestinal tract endoscopy.
Using the Healthcare Cost and Utilization Project (HCUP) statistics provided by the government for 2001, the number of people getting upper gastrointestinal endoscopy, which usually entails biopsy, was 697,675;
the number getting endarterectomy was 142,401; and
the number having coronary angiography was 719,949.13
Therefore, according to the JAMA study 17%, or 118,604 people had an unnecessary endoscopy procedure. Endarterectomy occurred in 142,401 patients; potentially 32% or 45,568 did not need this procedure. And 17% of 719,949, or 122,391 people receiving coronary angiography were subjected to this highly invasive procedure unnecessarily. These are all forms of medical iatrogenesis. [8]
The most recent controversy is reported in the New York Times:
“Spinal-fusion surgery is one of the most lucrative areas of medicine. An estimated half-million Americans had the operation this year, generating billions of dollars for hospitals and doctors. But there have been serious questions about how much the surgery actually helps patients with back pain and whether surgeons’ generous fees might motivate them to overuse the procedure.
Those concerns are now heightened by a growing trend among some surgeons to profit in yet another way — by investing in companies that make screws and other hardware they install.” [10]
Now, added to concerns about medicine’s low level of musculoskeletal training and these dangerous statistics, now we have to wonder if the orthopedist might be motivated to install 6 of those $1000 screws to your spine just because they are a stockholder of a lucrative medical device manufacturing company. [10]
The sanest and safest approach is to use conservative approaches like chiropractic care first. You can always resort to drugs or surgical approaches as a last-ditch resort, but the statistics suggest that most low back and neck pain can be successfully managed with lower costs and higher patient satisfaction by chiropractors.
You may want to explore research supporting chiropractic care for a wide variety of conditions in our Research section. There is also a significant body of work demonstrating the vastly superior Cost-Effectiveness of Chiropractic, as well as contrasting Patient Satisfaction With Chiropractic with standard Medical Care for the same conditions.
And Now Medicine Has Upped the Ante
Thanks to ChiroACCESS for the following commentary:
There is a lack of evidence-based support for the efficacy of complex fusion surgeries over conservative surgical decompression for elderly stenosis patients. There is, however, a significant financial incentive to both hospitals and surgeons to perform the complex fusions. Spinal stenosis is the most frequent cause for spinal surgery in the elderly. There has been a slight decrease in these surgeries between 2002 and 2007. However, there has also been an overall 15-fold increase in the more complex spinal fusions (360 degree spine fusions). [11]
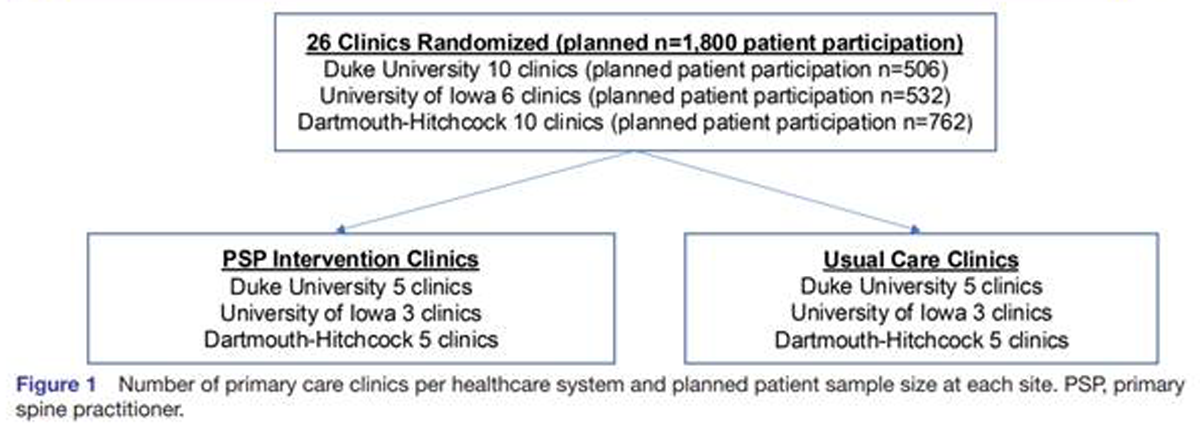
Deyo et. al., in yesterday’s issue of the Journal of the American Medical Association (April 7, 2010) concludes that:
“It is unclear why more complex operations are increasing. It seems implausible that the number of patients with the most complex spinal pathology increased 15-fold in just 6 years. The introduction and marketing of new surgical devices and the influence of key opinion leaders may stimulate more invasive surgery, even in the absence of new indications… financial incentives to hospitals and surgeons for more complex procedures may play a role…” There is a significant difference in mean hospital costs for simple decompression versus complex surgical fusion.
The cost of decompression is $23,724 compared to an average of $80,888 for complex fusion. [11]
Read the rest of this fascinating review at ChiroACCESS
You may also want to review:
REFERENCES:
- US Congressional House Subcommittee Oversight Investigation
Cost and Quality of Health Care: Unnecessary Surgery.
Washington, DC: Government Printing Office, 1976 - Herman R. Back Surgery.
Washington Post [Health Section], April 18, 1995 - Testimony to the Department of Veterans Affairs’ Chiropractic Advisory Committee
George B. McClelland, D.C., Foundation for Chiropractic Education and Research March 25, 2003 - Incidence of Adverse Drug Reactions in Hospitalized Patients: A Meta-analysis of Prospective Studies
JAMA 1998 (Apr 15); 279 (15): 1200-1205 - Nosocomial Infection Update
Emerg Infect Dis 1998 (Jul); 4 (3): 416-420 - Error in Medicine
JAMA 1994 (Dec 21); 272 (23): 1851-1857 - Medication errors in hospitalized cardiovascular patients
Arch Intern Med 2003 (Jun 23); 163 (12): 1461-1466 - Death by Medicine
LE Magazine March 2004 - Failed Back Surgery Syndrome: Diagnostic Evaluation
Journal of the American Academy of Orthopaedic Surgeons 2006 (Sep); 14 (9): 534-543 - The Spine as Profit Center
New York Times ~ December 30, 2006 - Money and Spinal Surgery: What Happened to the Patient?
ChiroACCESS April 8, 2010




I think the perception, in the general public, is that surgery must cure everything because it is surgery. I have seen too many times people going for an MRI and finding a disc bulge that is assumed to be causing all the pain therefore it must be operated on. I wonder how many back surgery patients were told that even after the spinal surgery they would need conservative rehabilitation, which they could do before the op to see if it made them better.
There will be those that require spinal surgery, but they must earn it first.
Some surgeons know and admit that spinal surgery is not cure that patients are looking for and explain these shortcomings to patients (you bet I surprised when I first spoke to them). I have began working with two spinal surgeons in the past few month here in Singapore. Even when working in private practice they are in my mind giving out honest information to their patients and have referred many of their patients for my care instead.
They also know that even if they remove a disc herniation that needs surgical attention proper follow up rehabilitation is needed.
I would like to see the statistics on failed back surgery. Almost every patient I talk to is deathly afraid of spinal fusions because they know someone who has had the surgery and now has greater pain than before the operation.
The problem I see is that there is tremendous muscle spasm generated by the fusion, probably because of the lack of movement.
[…] Originally posted here: ChiroOrg Blog – For Chiropractic and Chiropractors. “Why Do Spinal Surgery Rates Continue To Rise?” […]
@ Michael – I think you’re right on about the muscle spasm. Another thing I’m sure that contributes is the scar tissue that is produced from the surgery.
[…] New Study Suggests That Back Surgery Fails 74% of the Time ~ Chiro.Org Blog Editorial ~ October 22, 2010 […]
[…] Why Do Spinal Surgery Rates Continue To Rise? Chiro.Org Blog Editorial ~ April 10th, […]
Back surgery fails 74 percent of the time and yet insurers still cover the procedures and patients still line up for them hoping they want a quick fix. What they too often end up with is a problem that is much worse. Failed back surgery syndrome is “characterized by intractable pain and varying degrees of functional incapacitation occurring after spine surgery”. Where is the logic?
I often wonder if it’s just my perspective as a chiropractor that makes me believe that surgeries are a poor option. I hope that this helps surgeons and patients to make more careful decisions. I see so many patients that would jump at the chance to have surgery, thinking that it is the answer for anything and everything.
At the same time, the perception of a lot chiropractors is that adjustments can help anything and everyone. Wouldn’t it be great if there was an easy way to determine who needs surgery and who doesn’t?
On with the clinical trials!
RESPONSE from Frank:
The new European Guidelines for the Management of Acute and Chronic Nonspecific Low Back Pain specifically states:
“Surgery for non-specific CLBP cannot be recommended unless 2 years of all other recommended conservative treatments — including multidisciplinary approaches with combined programs of cognitive intervention and exercises — have failed”.
[…] to the data publicly available at Chiro.org (Why Do Spinal Surgery Rates Continue To Rise), it is estimated that in 1995 more than 250.000 lower back surgeries were performed, costing the […]
[…] Why Do Spinal Surgery Rates Continue To Rise? Chiro.Org Blog Editorial ~ April 10th, […]