Conservative Chiropractic Management of Urinary Incontinence Using Applied Kinesiology: A Retrospective Case-series Report
SOURCE: J Chiropr Med. 2012 (Mar); 11 (1): 49–57 ~ FULL TEXT
Scott C. Cuthbert and Anthony L. Rosner
Chief Clinician, Chiropractic Health Center, PC, Pueblo, CO 81004
OBJECTIVE: The purpose of this case series is to describe the chiropractic management of 21 patients with daily stress and occasional total urinary incontinence (UI).
CLINICAL FEATURES: Twenty-one case files of patients 13 to 90 years of age with UI from a chiropractic clinic were reviewed. The patients had a 4-month to 49-year history of UI and associated muscle dysfunction and low back and/or pelvic pain. Eighteen wore an incontinence pad throughout the day and night at the time of their appointments because of unpredictable UI.
INTERVENTION AND OUTCOME: Patients were evaluated for muscle impairments in the lumbar spine, pelvis, and pelvic floor and low back and/or hip pain. Positive manual muscle test results of the pelvis, lumbar spine muscles, and pelvic floor muscles were the most common findings. Lumbosacral dysfunction was found in 13 of the cases with pain provocation tests (applied kinesiology sensorimotor challenge); in 8 cases, this sensorimotor challenge was absent. Chiropractic manipulative therapy and soft tissue treatment addressed the soft tissue and articular dysfunctions. Chiropractic manipulative therapy involved high-velocity, low-amplitude manipulation; Cox flexion distraction manipulation; and/or use of a percussion instrument for the treatment of myofascial trigger points. Urinary incontinence symptoms resolved in 10 patients, considerably improved in 7 cases, and slightly improved in 4 cases. Periodic follow-up examinations for the past 6 years, and no less than 2 years, indicate that for each participant in this case-series report, the improvements of UI remained stable.
CONCLUSION: The patients reported in this retrospective case series showed improvement in UI symptoms that persisted over time.
From the Full-Text Article:
Introduction
Urinary incontinence (UI) occurs when there is leakage of urine involuntarily, most commonly in older patients. [1] Fantl et al [2] state that incontinence affects 4 of 10 women and 1 of 10 men during their lifetime, and about 17% of children younger than 15 years. A large postpartum study of the prevalence of UI found that 45% of women experienced UI at 7 years postpartum. Thirty-one percent who were initially continent in the postpartum period became incontinent in the future. [3]
Continence depends primarily on the adequate function of 2 muscular systems — the urethral muscular support system and the sphincteric muscular network of the pelvic floor muscles (PFM). [4] These systems include the levator ani muscle, detrusor muscle, and pelvic floor muscles (coccygeus, obturator externus, obturator internus, gemellus inferior, gemellus superior, and levator ani), as well as the pudendal nerve that emerges from the sacral plexus. The striated muscles of the pelvic floor play an integral role in the closure of the lumen of the urethra and the maintenance of continence. [5] In women with stress UI, ineffective contraction or control of the pelvic floor muscles permits descent of the bladder neck with inadequate closure of the urethra, resulting in the leakage of urine. [6]
The comorbidities of lumbopelvic pain, incontinence, and breathing pattern disorders are slowly being elucidated. [7, 8] Musculoskeletal impairments, and specifically muscular imbalances between agonist and antagonist muscles in the pelvis, create articular strain and soft tissue stresses that can lead to pain and UI. [9]
Current observations suggest that patients with stress incontinence may have imbalances in several lumbopelvic muscles that inhibit the PFM and lead to incontinence. [10] Recent data also indicate that breathing difficulties and incontinence are associated with increased chances for the development of low back pain, [11] demonstrating that the interactions between the lumbar and pelvic muscles and joints may be an important consideration in cases of UI.
A recent study assessed strength changes in the PFM using a perineometer (a pressure electromyograph that registers contractions of the PFM) after the application of chiropractic manipulative therapy (CMT). This investigation showed that phasic perineal contraction and basal perineal tonus, force, and pressure increased after CMT. [12] The duration of these force changes will have to be assessed in subsequent studies of this type.
It was Arnold Kegel [13] who first advocated pelvic floor muscle strengthening and retraining for stress incontinence, indicating his recognition of the importance of muscle inhibitions in cases of UI. Kegel’s program of strengthening the inhibited muscles of the pelvic floor has shown some promise. [14-17] The potential usefulness of the applied kinesiology manual muscle test (AK MMT) approach in this model would be the identification of the inhibited muscles involved and the therapeutic approaches used to immediately address these inhibitions with CMT. A number of other reports have been made on the use of CMT for elderly patients with UI. [18] Stude et al [19] reported a case study of a 14-year-old female adolescent treated with CMT who recovered completely from traumatically induced UI. The applied kinesiology (AK) approach to a postappendectomy-induced case of UI has been described as well. [20] Chiropractic manipulative therapy has been shown to be effective in other reports on bladder control problems. [21-23]
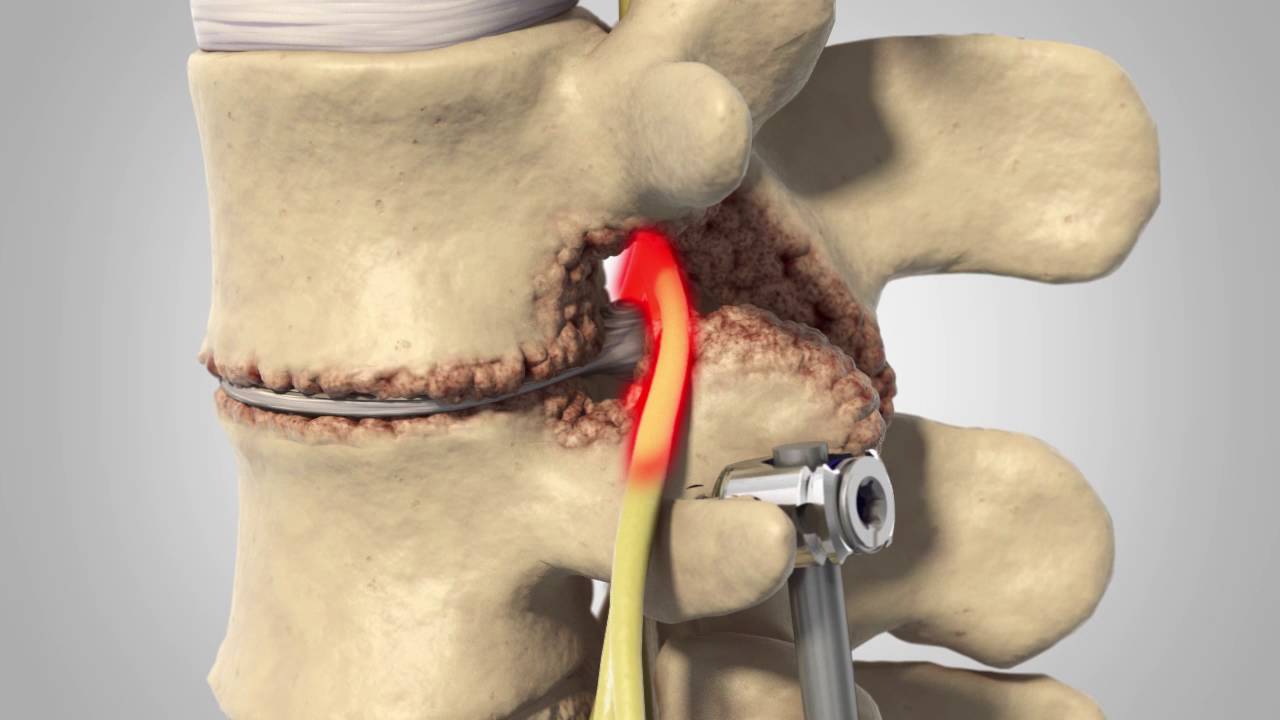
Lumbar and sacral nerve root compression as the result of lumbar and sacral articular dysfunction and degeneration has been identified as a potential cause of pelvic pain and organic dysfunction, a term coined by Browning. [24, 25] It is hypothesized that there may be a relationship between lumbar and pelvic muscles and UI.
The purpose of this case series is to report on the findings of chiropractic management of patients with UI. The patients included in this report presented for chiropractic treatment of either UI directly or another condition, with their UI being disclosed during the initial history taking at the beginning of treatment. Each patient signed informed, written consent forms to be examined and treated and to be included in this case-series report.
Discussion
This review of 21 cases of UI has suggested that there may be a relationship between MMT of the pelvic and lumbar spinal muscles (particularly the PFM), as this seemed to be consistent in each of the selected cases.
The following is a discussion of some of the theories that may explain this relationship. The PFM run from the pubic symphysis to the ischial spines bilaterally. These muscles and fascia continue superiorly, with the myofascia surrounding the pelvic organs and ligaments of the pelvic joints. The PFM are also continuous with the abdominal muscles and play a role in urological function. [38, 39] The PFM are linked to the hips and obturator internus muscles; and thus, it is likely that the functional PFM extend from greater trochanter to greater trochanter. [40, 41] If the PFM are hypotonic (as they were in 14 cases of this report), the bladder and other pelvic organs may tend toward prolapse and descend toward their orifices.
Scars from pregnancy, cesarian deliveries, and one appendectomy may possibly disturb the respiratory mechanics of the oblique abdominal and diaphragm muscles, resulting in physical discomfort and incontinence. As well, presence of incontinence may cause emotional stress. The use of incontinence pads may also increase anxiety, [42] producing breathing pattern disorders that may further disturb diaphragm muscle function. Breathing pattern disorders are vulnerable to emotional distress, muscle imbalances, and pain. [43]
The patients in this study showed breathing pattern disorders that may have been associated with weakness in the rectus abdominus (cases 10-14 and 17) or diaphragm muscles (cases 1-4, 8, and 11) during MMT examination (except for cases 5 and 7 who had abdominal scars but no MMT weakness in these 2 muscles). These factors may have combined to affect the diaphragm muscle’s function, which has been connected to the function of the pelvic floor, bladder, and urethra. [4-6]
Soft tissue treatment of these scars was done using a percussor instrument. It is thought that the immediate effect of percussion modifies the physical nature of the myofascial matrix. [44] Percussion may also press fluid from the nuclear bag of the muscle spindle cells (part of the MTrPs pathophysiology), reducing the tension in the capsule of the spindles. [45]
There is also a theory that the PFM group should co-contract with the rectus abdominus muscle. [46] The examination findings in this report showed that where the rectus abdominus (10 cases) or PFM (14 cases) were inhibited, one member of this force couple may have disturbed the other when dysfunctional.
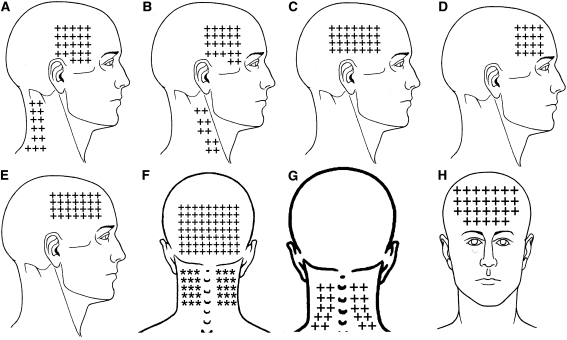
Travell and Simons [47] state that “weakness is generally characteristic of muscles with active MTrPs.” This weakness may also be present in cases of incontinence in the urethral and sphincteric muscular support systems (including the levator ani, detrusor, and pelvic floor muscles) of the lower pelvis. [3, 4, 39] A positive response to pincer palpation of the PFM was present in 11 of the cases (1-2, 3, 7, 9-13, and 15-16), indicating the possibility that MTrPs played some role in the PFM inhibitions found. Pelvic floor muscle imbalances have been noted by some researchers to be frequently associated with sacroiliac dysfunction. [48]
Kobesova et al [49] suggest that scars may develop adhesive properties that disturb tissue tension, alter proprioceptive input, and create functional changes similar to active MTrPs. Moncayo and Moncayo [50] have recently demonstrated the usefulness of the AK treatment of scars upon muscular function.
Scars from previous surgeries may form connective tissue MTrPs. [51] The theory of active MTrPs in the abdominal muscles beneath the scars was investigated using the AK methods of pincer palpation and the muscle stretch reaction. [33, 34, 37] Both of these tests identified the presence of active MTrPs in the patients of this report. Travell and Simons [47] describe the method of diagnosis and treatment of MTrPs (called pincer palpation and percussion) used in this report.
The aforementioned observations of Kobesova et al, [49] Moncayo and Moncayo, [50] and Travell and Simons [51] may relate to the findings of Arnold Kegel, who first advocated pelvic floor muscle strengthening and retraining for stress incontinence. [47] It should be observed that in cases like these where muscle inhibition of the PFM played some role in the UI, Sherrington’s [52] law of reciprocal innervation (“when one muscle contracts, it’s direct antagonist relaxes to an equal extent”) suggests that some of the PFM—antagonists to the inhibited PFM—may already be hypertonic. Therefore, toning exercises for the PFM may be counterproductive.
The AK MMT is theorized to have identified the inhibited PFM or the inhibited muscles related to the PFM anatomically or functionally. The AK sensorimotor challenge then rapidly diagnosed the manipulable articulation or soft tissue producing this inhibition. During the examination, this sensorimotor challenge produced an immediate strengthening of the PFM or muscle(s) related to the pelvic floor. Treatment to the articulation or soft tissue (guided by the AK sensorimotor challenge) led to the immediate — and in 10 cases long-lasting—strengthening of the PFM or muscle related to the pelvic floor anatomically or functionally. From these considerations, there may be reason to suspect that the patterns of muscle weakness associated with UI and disclosed by MMT methods may be of clinical utility in guiding CMT.
Conclusion
This report discussed a chiropractic treatment approach and the resolution, considerable improvement, or slight improvement of UI in 21 cases. Further research with defined inclusion criteria and validated outcome measures is needed to evaluate the effectiveness of CMT and AK procedures in managing UI.



Leave A Comment