Patients Receiving Chiropractic Care in a Neurorehabilitation Hospital: A Descriptive Study
SOURCE: J Multidiscip Healthc. 2018 (May 3); 11: 223–231
Robert D Vining, Stacie A Salsbury, W Carl Cooley, Donna Gosselin, Lance Corber, and Christine M Goertz
Palmer Center for Chiropractic Research,
Palmer College of Chiropractic,
Davenport, IA, USA.
OBJECTIVES: Individuals rehabilitating from complex neurological injury require a multidisciplinary approach, which typically does not include chiropractic care. This study describes inpatients receiving multidisciplinary rehabilitation including chiropractic care for brain injury, spinal cord injury (SCI), stroke, and other complex neurological conditions.
DESIGN: Chiropractic services were integrated into Crotched Mountain Specialty Hospital (CMSH) through this project. Patient characteristics and chiropractic care data were collected to describe those receiving care and the interventions during the first 15 months when chiropractic services were available.
SETTING: CMSH, a 62–bed subacute multidisciplinary rehabilitation, skilled nursing facility located in Greenfield, New Hampshire, USA.
RESULTS: Patient mean (SD) age (n=27) was 42.8 (13) years, ranging from 20 to 64 years. Males (n=18, 67%) and those of white race/ethnicity (n=23, 85%) comprised the majority. Brain injury (n=20) was the most common admitting condition caused by trauma (n=9), hemorrhage (n=7), infarction (n=2), and general anoxia (n=2). Three patients were admitted for cervical SCI, 1 for ankylosing spondylitis, 1 for traumatic polyarthropathy, and 2 for respiratory failure with encephalopathy. Other common comorbid diagnoses potentially complicating the treatment and recovery process included myospasm (n=13), depression (n=11), anxiety (n=10), dysphagia (n=8), substance abuse (n=8), and candidiasis (n=7). Chiropractic procedures employed, by visit (n=641), included manual myofascial therapies (93%), mechanical percussion (83%), manual muscle stretching (75%), and thrust manipulation (65%) to address patients with spinal-related pain (n=15, 54%), joint or regional stiffness (n= 14, 50%), and extremity pain (n=13, 46%). Care often required adapting to participant limitations or conditions. Such adaptations not commonly encountered in outpatient settings where chiropractic care is usually delivered included the need for lift assistance, wheelchair dependence, contractures, impaired speech, quadriplegia/paraplegia, and the presence of feeding tubes and urinary catheters.
CONCLUSION: Patients suffered significant functional limitations and comorbidity resulting in modifications to the typical delivery of chiropractic care. Chiropractic services focused on relieving musculoskeletal pain and stiffness.
KEYWORDS: chiropractic; integrative medicine; rehabilitation; spinal cord injury; stroke
From the Full-Text Article:
Introduction
Persons suffering spinal cord injury (SCI), brain injury, or stroke with complicated sequela typically require multidisciplinary rehabilitation due to complex multisystem effects. [1–3] Over 3,000 cases of acute SCIs occur within the USA each year [4] as do an estimated 795,000 cerebrovascular accidents (stroke). [5] Of the estimated 2.5 million annual emergency department visits for traumatic brain injury (TBI), the US Centers for Disease Control and Prevention estimates ~280,000 persons are hospitalized for moderate to severe injury. [6] Healthcare costs to manage moderate to severe TBI are more than US$13 billion annually. [7] Individuals recovering from acquired brain injury and SCI often experience limitations in physical mobility and activities of daily living, impaired cognition, psychological conditions, and chronic pain, which can lead to permanent institutionalization. [5, 7, 8] Many patients with such complex neurological conditions are admitted to post-acute rehabilitation settings or skilled nursing facilities to support their recovery process. [5]
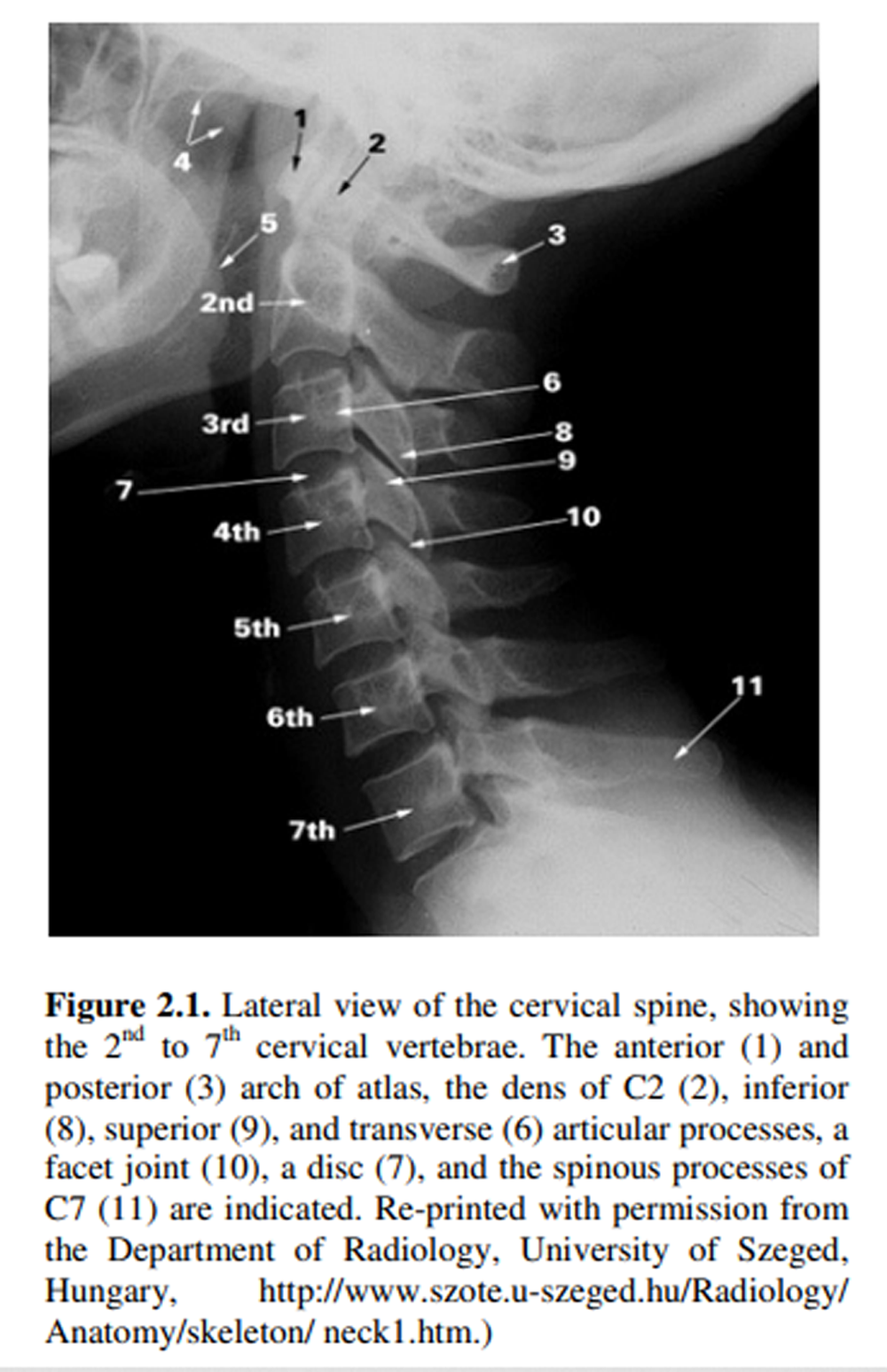
Many factors can impede rehabilitation from complex neurological conditions including the presence of comorbidities such as pain, depression, cardiopulmonary disease, gastrointestinal disorders, substance abuse disorder, and musculoskeletal symptoms. [9–11] Hemiplegic shoulder pain, a common poststroke disorder, is caused by several possible underlying pathologies that can significantly interfere with movement and sleep and contribute to delayed functional recovery. [12] Individuals with SCI commonly experience spasticity, poor posture, and upper extremity overuse, which contribute to persistent musculoskeletal pain. [13, 14] Common conditions associated with brain injury include co-injury from polytrauma, headache from multiple etiologies, and cognitive changes that complicate both clinical assessment and treatment response. [15, 16]
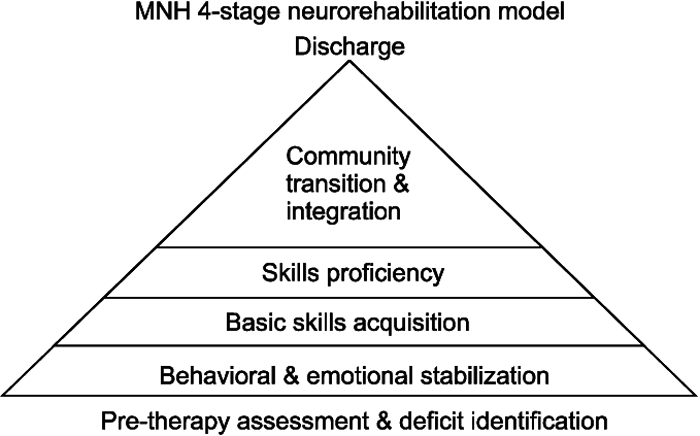
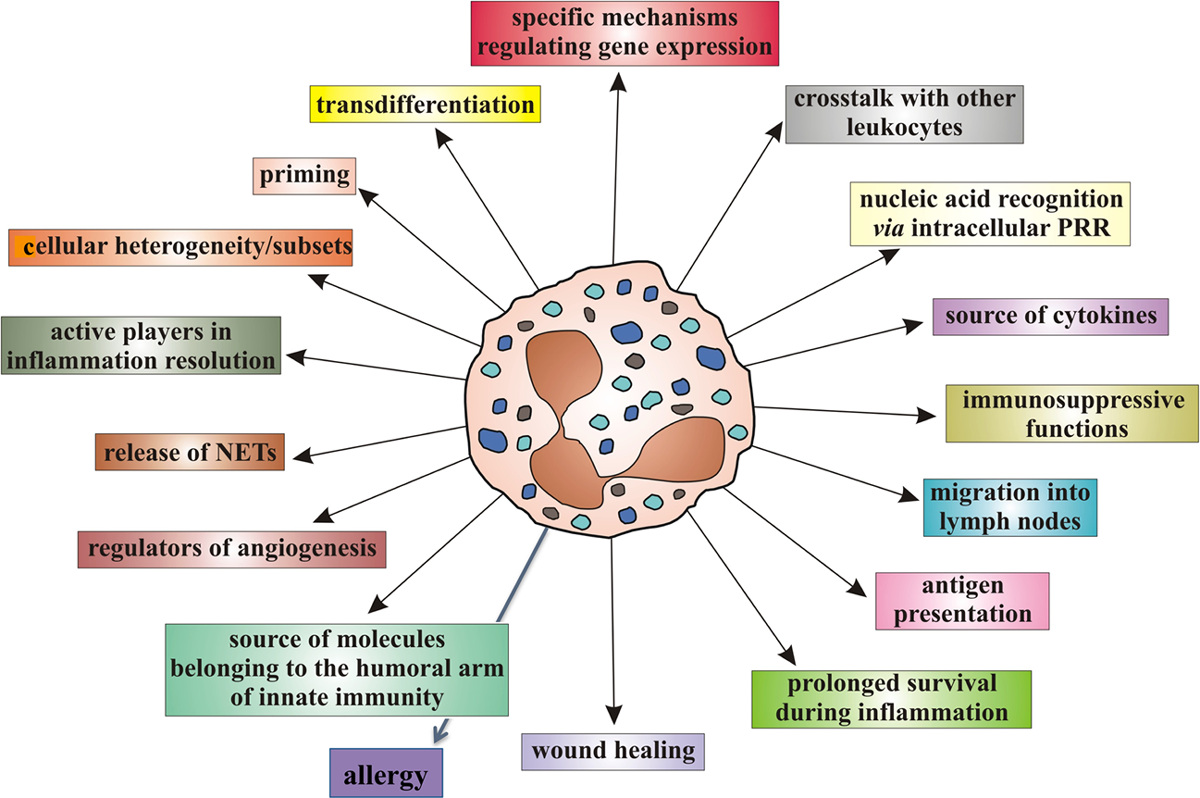
Rehabilitation-focused disciplines, such as physical, occupational, and speech therapies, support inpatients recovering from and adapting to complex neurological injury. Chiropractic services may also offer a positive contribution. Spinal manipulation, a therapy commonly used by doctors of chiropractic (DCs), is known to influence pain through complex central nervous system mechanisms. [17] Evidence suggests other manual therapies commonly used by DCs also generate complex neurological response cascades leading to clinical improvement. [18] Some of these interventions show promise for reducing pain in patients recovering from SCI. [19] Because chiropractic services are integrated increasingly into outpatient multidisciplinary environments where nonpharmacological interventions are needed or preferred, [20–24] exploring care that can be delivered in inpatient settings is a next logical step. [25]
Currently, little is known about chiropractic service delivery within the inpatient neurorehabilitation context. However, such knowledge is vital to informing integration decisions. Barriers to more widespread integration include a lack of utilization and cost data for the specific environment, [26] perceived loss of autonomy for the chiropractic provider, [27, 28] and unfamiliarity with how chiropractic procedures can complement other treatments. [29–31] The purpose of this study was to describe the clinical characteristics, chiropractic service utilization patterns, and common care challenges among patients with complex neurological conditions receiving subacute inpatient care including chiropractic at a rehabilitation specialty hospital.
Read the rest of this Full Text article now!



Leave A Comment