A Risk-benefit Assessment Strategy to Exclude Cervical Artery Dissection in Spinal Manual-therapy: A Comprehensive Review
SOURCE: Annals of Medicine 2019 (Mar 19): 1–10 [Epub]
Aleksander Chaibi & Michael Bjørn Russell
Head and Neck Research Group,
Research Centre, Akershus University Hospital,
Oslo, Norway.
Cervical artery dissection refers to a tear in the internal carotid or the vertebral artery that results in an intramural haematoma and/or an aneurysmal dilatation. Although cervical artery dissection is thought to occur spontaneously, physical trauma to the neck, especially hyperextension and rotation, has been reported as a trigger. Headache and/or neck pain is the most common initial symptom of cervical artery dissection. Other symptoms include Horner’s syndrome and lower cranial nerve palsy. Both headache and/or neck pain are common symptoms and leading causes of disability, while cervical artery dissection is rare. Patients often consult their general practitioner for headache and/or neck pain, and because manual-therapy interventions can alleviate headache and/or neck pain, many patients seek manual therapists, such as chiropractors and physiotherapists. Cervical mobilization and manipulation are two interventions that manual therapists use. Both interventions have been suspected of being able to trigger cervical artery dissection as an adverse event. The aim of this review is to provide an updated step-by-step risk-benefit assessment strategy regarding manual therapy and to provide tools for clinicians to exclude cervical artery dissection.
| Key messages |
-
Cervical mobilization and/or manipulation have been suspected to be able to trigger cervical artery dissection (CAD). However, these assumptions are based on case studies which are unable to established direct causality.
There are more articles like this @ our:
-
The concern relates to the chicken and the egg discussion, i.e. whether the CAD symptoms lead the patient to seek cervical manual-therapy or whether the cervical manual-therapy provoked CAD along with the non-CAD presenting complaint.
-
Thus, instead of proving a nearly impossible causality hypothesis, this study provide clinicians with an updated step-by-step risk–benefit assessment strategy tool to
(a) facilitate clinicians understanding of CAD,
(b) appraise the risk and applicability of cervical manual-therapy, and
(c) provide clinicians with adequate tools to better detect and exclude CAD in clinical settings.
KEYWORDS: Cervical artery dissection; carotid artery dissection; manipulation; manual-therapy; stroke; vertebral artery dissection
From the FULL TEXT Article:
Introduction
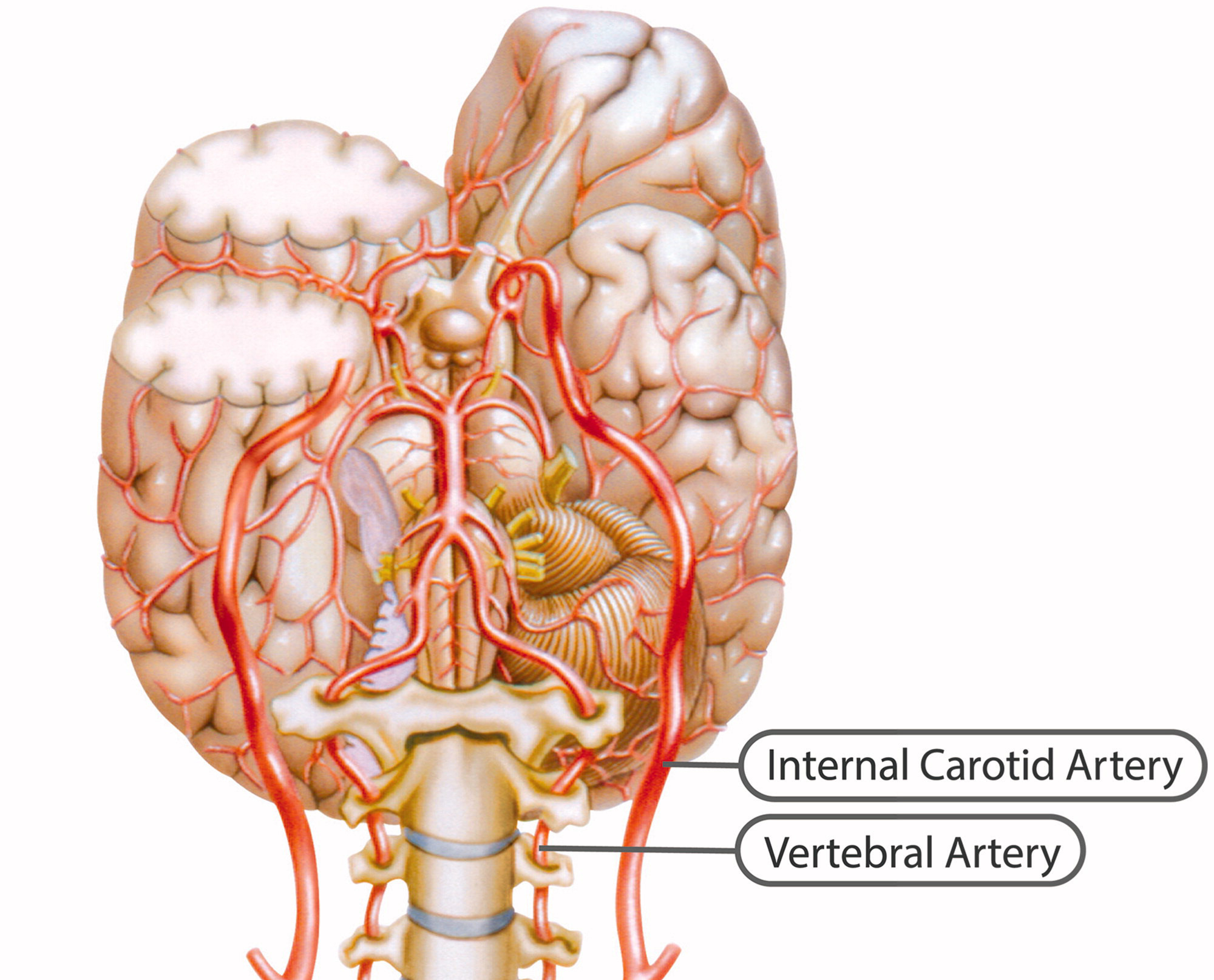
Cervical artery dissection (CAD) refers to a tear in the internal carotid artery (ICA) or the vertebral artery (VA), resulting in an intramural haematoma and/or an aneurysmal dilatation, which can ultimately be detrimental to the individual. The pathophysiology of CAD is not fully understood, but multiple coexisting pathological processes leading to a predisposing weakness of the arterial wall, namely, a large aortic root diameter, increased stiffness of the carotid wall, material and circumferential wall stress, hypertension, endothelial dysfunction, and arterial redundancies, have been proposed to increase the risk of CAD. [1]
Fortunately, the incidence rate of CAD is relatively low, estimated at 2.9/100,000 individuals per year in the general population. [2] Internal carotid artery dissections (ICADs) occur approximately 3–5 times more frequently than vertebral artery dissections (VADs). [3, 4] This corresponds to 9476 new American CAD cases and 21,537 new European CAD cases per year. CAD usually only occurs once.
Ischaemic stroke is the most common clinical symptom in CAD, and the risk of subarachnoid haemorrhage (SAH) is greater in intracranial artery dissection than in CAD. [5] However, there is also a selection bias towards those with CAD without subarachnoid haemorrhage being recruited through neurology departments, whereas recruitment through departments of neurosurgery or interventional neuroradiology is biased towards CAD with SAH [5]. A French prospectively neurological department study in tertiary health care found clinical symptoms to occur in 156 (92%) of 169 patients with spontaneous VAD, i.e. stroke in 114 (67%), TIA in 17 (10%), and occipital head and/or neck pain alone in 21 (12%) patients, SAH without ischaemia were found in three (2%) patients, and sensorimotor cervical radiculopathy C5/C6 in one patient (1%). Three of the patients with ischemic stroke also showed signs of SAH on brain imaging. [6] A Swiss prospectively neurological department study in tertiary health care found clinical symptoms to occur in 290 (97%) of 298 patients with spontaneous ICAD, i.e. stroke in 165 (55%), TIA in 37 (12%), amaurosis fugax in 8 (3%), local symptoms, and signs (headache, neck pain, Horner’s syndrome and nerve palsy) in 80 (27%), while eight (3%) were asymptomatic. [7]
The prognosis of disability after CAD at 3 months is good for 89% of cases, with 91% for ICAD and 88% for VAD, according to the modified Rankin score (mRS 0–2): (0) no symptoms, (1) no significant disability despite symptoms and able to carry out all usual duties and activities, and (2) slight disability, unable to carry out all previous activities, but able to look after own affairs without assistance. [2, 8] The mortality rate is less than 4% [1, 4]: mean 5.1% (SD 7.2) for ICAD [2, 9–21] and mean 1.3% (SD 2.3) for VAD [2, 14, 16, 18, 20–22], calculated by the authors. The mean age of CAD patients is 44 years (46 years for men and 41 years for women [23], with a slight male preponderance (55%). [24] CAD is extremely rare in children and adults beyond the age of 65 years. [25]
Headache and/or neck pain are the most common initial symptoms of CAD. [26] Other symptoms are Horner’s syndrome and lower cranial nerve palsy. [4] The headache is often new and unilateral, exhibits sudden onset, and may resemble a migraine or cluster headache. [27] The time from initial symptoms to ischaemic stroke varies from minutes to few weeks. [28]
Read the rest of this Full Text article now!

Leave A Comment